Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Chronic Nonbacterial Osteomyelitis (CNO) is an autoinflammatory disorder of bone usually beginning in children between the ages of 7-12. It typically affects metaphyses of the long bones, vertebral bodies, and the clavicle. Although, any bone can be affected, involvement of the skull is extremely uncommon. The objectives of our study are to 1) illustrate presenting features associated with CNO of the temporal bone, its treatment, & response to therapy. 2) Increase awareness that CNO can involve the temporal bone to facilitate earlier diagnosis and treatment.
Methods: Patients diagnosed with CNO between June 2002-May 2022 at The Hospital for Sick Children were identified by searching Bialogics,TM the Electronic Medical Records Epic, and Chart Maxx. Charts were searched for the term “skull” to identify cases. To obtain records prior to 2018 (prior to the Epic electronic medical record) we ran a word search of pertinent synonyms to identify cases of CNO involving the temporal bone in the ISYS word text search program. Research Ethics Board approval was obtained for this study.
Results: Three cases of CNO affecting the petrous temporal bone were identified. All had been previously diagnosed with CNO. Age of onset of CNO was 2.3 to 9 years of age; all were female (Table 1). Time from CNO diagnosis to onset of petrous bone lesions ranged from 6-17 months. Two patients developed a Bell’s Palsy and hearing loss. All patients were treated with a non-steroidal anti-inflammatory drug (NSAID) and the one patient with hearing loss also received anti-TNF therapy (adalimumab) and responded well with resolution of hearing loss. The other patient received NSAID therapy and has persistent bilateral hearing loss, in the context of recurrent otitis media.
Conclusion: The skull is rarely involved in CNO, with ~1% of patients presenting with lesions in the frontal bone. Temporal bone involvement has rarely been reported with only two cases to our knowledge . It is unknown why CNO rarely affects the skull. One presumption is that CNO tends to affect the metaphyses and epiphyses of the long bones which the skull does not have, although, the pelvis also does not have a metaphysis and is a common site for CNO lesions. Another thought is the increased metabolic activity and blood supply at the epiphysis with chondrocyte maturation could result in increased propensity of immune dysregulation and inflammatory lesions. With less osteo metabolic activity the risk of dysregulation may be less. Interestingly all three cases developed skull involvement while on treatment for CNO.There is no standardized treatment for CNO. Consensus guidelines provide options including non-steroidal anti-inflammatories (first line), glucocorticoids, disease modifying drugs (methotrexate, sulfasalazine), Tumor Necrosis Factor (TNF) inhibitors with or without methotrexate, and bisphosphates (pamidronate or zolendronic acid). In case one anti-TNF therapy was used due to the severity of hearing loss. CNO is challenging to diagnose, with 7% of patients being diagnosed five years after symptom onset. It is important to consider CNO on the differential in patients who present with cranial nerve abnormalities, hearing loss, and those with presumed infectious osteomyelitis.
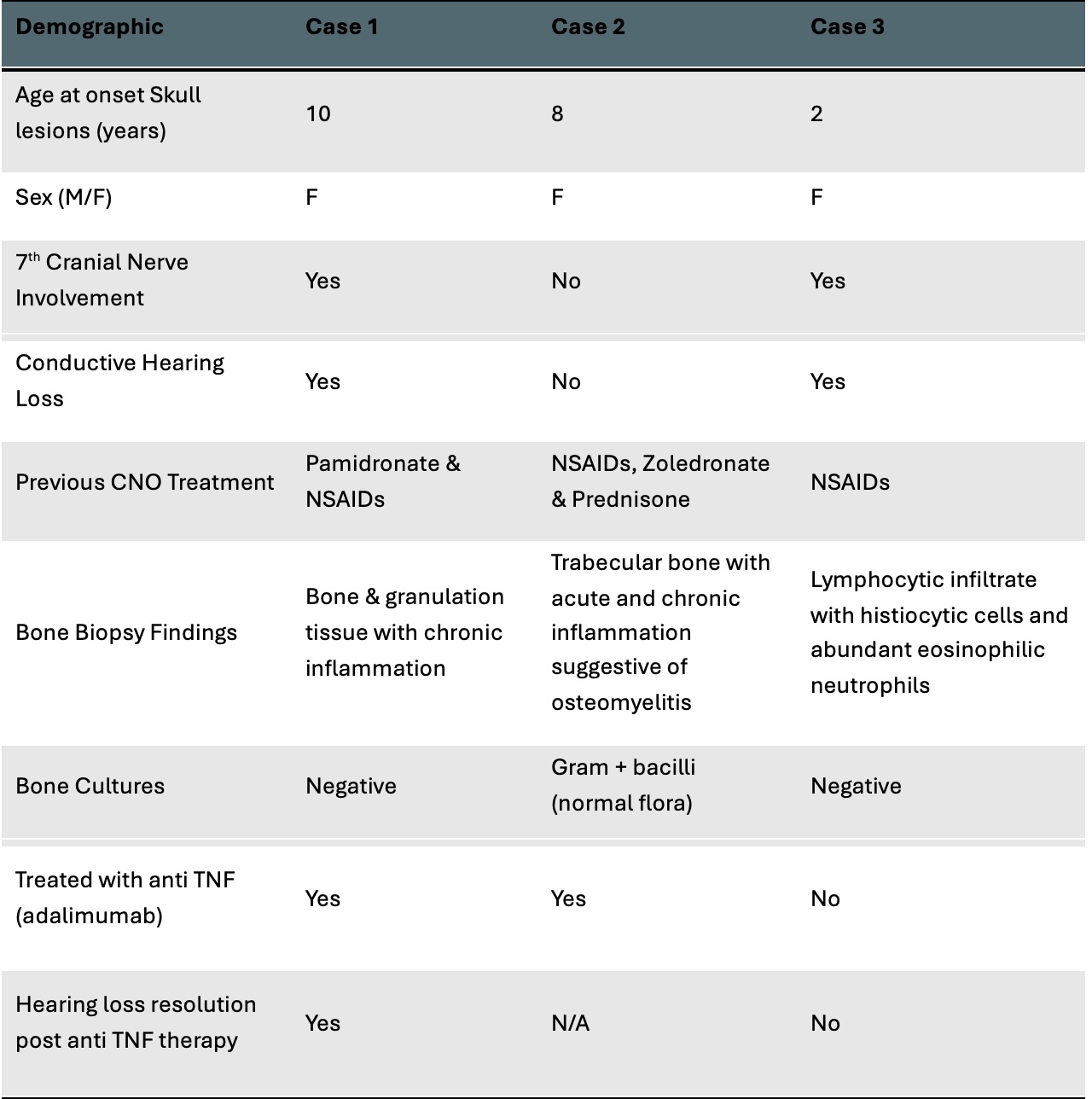 Figure 1: Case 1 Right Temporal Bone Erosion
Figure 1: Case 1 Right Temporal Bone Erosion
To cite this abstract in AMA style:
McColl J, Goh I, Branson H, Peralta K, Aeenfar D, Cushing S, Schneider R, laxer R. Chronic Non-Bacterial Osteomyelitis of the Petrous Bone: A Case Series [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/chronic-non-bacterial-osteomyelitis-of-the-petrous-bone-a-case-series/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/chronic-non-bacterial-osteomyelitis-of-the-petrous-bone-a-case-series/

.jpg)