Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoarthritis (OA) is a leading cause of disability and pain in older adults. While not traditionally viewed as fatal, OA contributes significantly to morbidity and, in some cases, mortality. This study evaluates national mortality trends and demographic disparities associated with OA (ICD-10 M15–M19) from 1999 to 2020 using U.S. death certificate data.
Methods: Mortality data were extracted from the CDC WONDER Multiple Cause of Death database. Age-adjusted mortality rates (AAMRs) per 100,000 population were calculated using census-adjusted standard populations. Deaths were stratified by year, state, sex, 10-year age group, race/ethnicity, Hispanic origin, place of death, and urban-rural classification based on the 2013 NCHS scheme.
Results: From 1999 to 2020, there were 15,948 deaths attributed to osteoarthritis (OA) in the United States. The age-adjusted mortality rate (AAMR) declined by 75% over the study period, dropping from 0.31 per 100,000 in 1999 to 0.08 in 2020. Despite this progress, notable disparities remain. Females experienced nearly twice the mortality burden of males, with an AAMR of 0.25 compared to 0.14. Mortality rose steeply with advancing age, reaching 8.5 per 100,000 among adults aged 85 and older. Racial and ethnic differences showed the highest AAMRs among White (0.22) and Black (0.17) individuals, while Hispanic and Asian/Pacific Islander groups had lower rates at 0.10 and 0.06, respectively. AAMRs increased with rurality, ranging from 0.18 in large metropolitan areas to 0.30 in noncore rural regions. State-level variation was substantial, with AAMRs ranging from 0.08 in Hawaii to 0.66 in Vermont, highlighting a greater burden in rural and mountain states. Regarding place of death, 43.6% of OA-related deaths occurred in nursing homes or long-term care facilities, 23.4% in inpatient medical settings, and 22.2% in the decedent’s home.
Conclusion: Osteoarthritis mortality in the U.S. has declined significantly over the past two decades, likely reflecting improved awareness and comorbidity management. However, consistent disparities by age, sex, race, geography, and care setting underscore the unequal burden of this chronic disease. These findings highlight the need for targeted health policy and equitable access to supportive care, particularly in aging and rural populations.
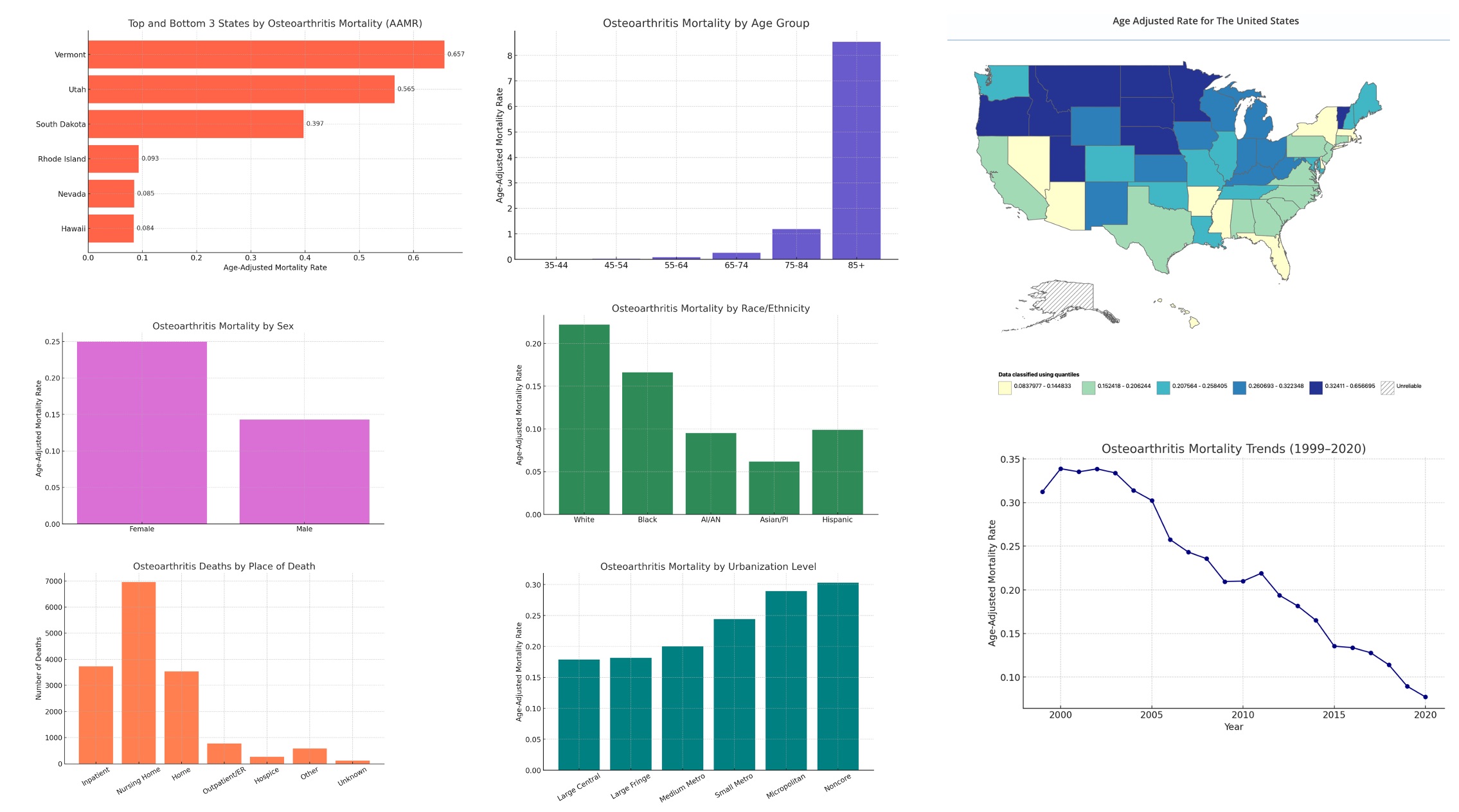 Graphs showing state, demographic, gender, race, age group, year, place of death, mortality from Osteoarthritis
Graphs showing state, demographic, gender, race, age group, year, place of death, mortality from Osteoarthritis
To cite this abstract in AMA style:
Makhoul G, Khalid A, Munshi H, Rajab I, Hussain M, John R, Assaf E, Al Badawy A, Khatiashvili B, Isshak R, Mateen N, Lahita R. Aging Unevenly: National Trends and Inequities in Osteoarthritis Mortality, 1999–2020 [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/aging-unevenly-national-trends-and-inequities-in-osteoarthritis-mortality-1999-2020/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/aging-unevenly-national-trends-and-inequities-in-osteoarthritis-mortality-1999-2020/
