Session Information
Date: Tuesday, October 28, 2025
Title: (2015–2051) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is common and important feature of systemic autoimmune rheumatic diseases (SARD). Rheumatologists and pulmonologists are central to the care of this complex condition. Specialists have unique training and expertise; whether these differences lead to distinct approaches to SARD-ILD treatment is unknown. We conducted a national, cross-sectional survey of rheumatologists and pulmonologists to assess how subspecialty affects physician management of SARD-ILD.
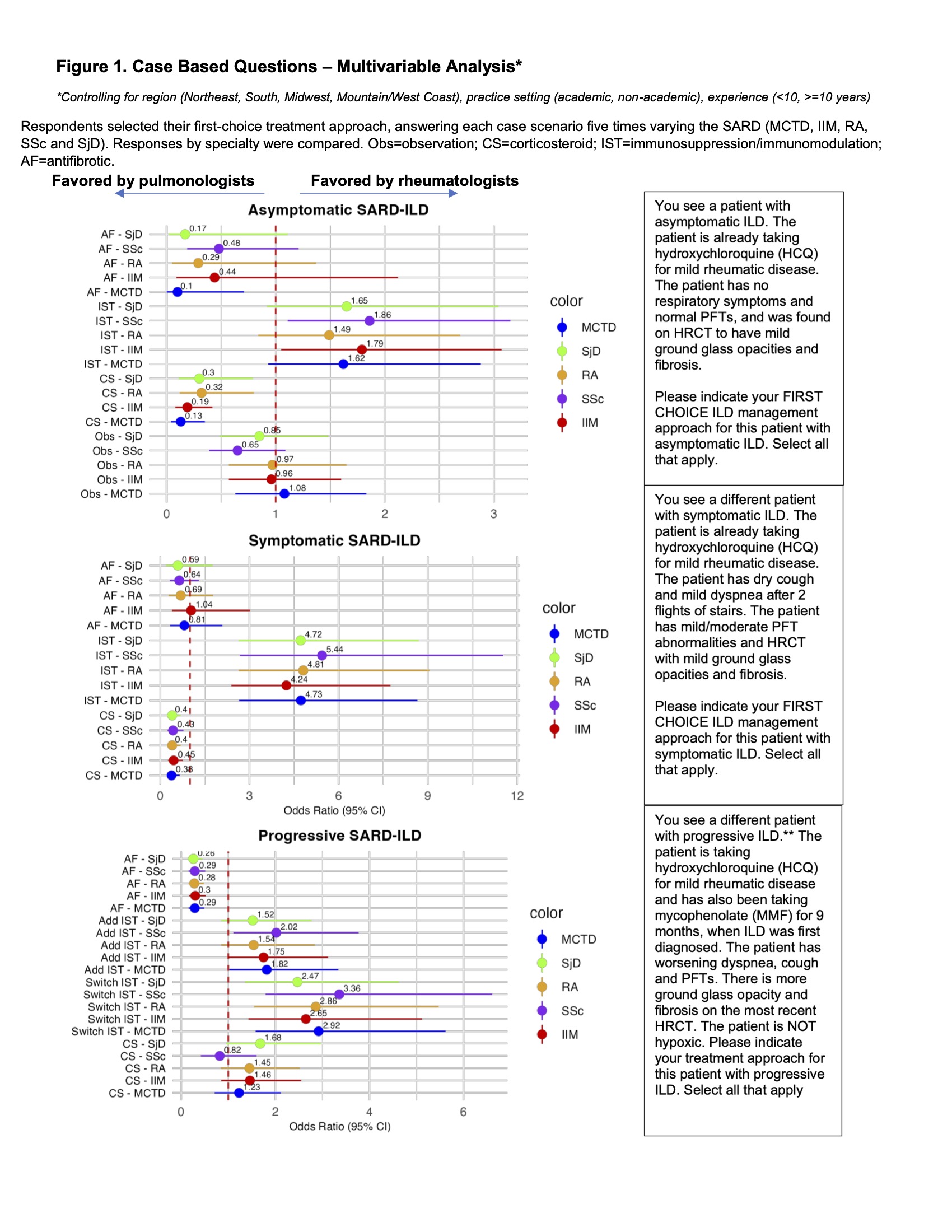
Methods: Surveys were electronically distributed to United States pulmonologists and rheumatologists identified through professional society memberships and social media. Surveys contained case questions on SARD-ILD management with variations of the underlying disease (mixed connective tissue disease, idiopathic inflammatory myopathy, rheumatoid arthritis, systemic sclerosis and Sjogren’s) and ILD severity (asymptomatic, symptomatic, progressive). Surveys also contained items on perceived importance of variables to treatment decisions, as well as opinions on ownership over aspects of management and healthcare maintenance. We analyzed responses submitted 5-9/2024.We compared specialists’ responses via univariate logistic regression, Chi-squared or Fisher’s exact tests; we performed multivariable logistic regression of case questions controlling for practice setting, clinical experience and geography.
Results: Analyses included 309 participants (rheumatologists=184, pulmonologists=125) (Table 1). Compared to rheumatologists, pulmonologists were more likely to treat asymptomatic and symptomatic ILD with corticosteroids for all SARD except asymptomatic systemic sclerosis (odds ratios [OR] 2.22-7.69, all p< 0.05), and progressive ILD with antifibrotics (OR 3.33-3.84, all p< 0.05). Compared to pulmonologists, rheumatologists were more likely to add or modify immunomodulation/immunosuppression for all symptomatic and progressive SARD-ILD (OR 1.82-5.44, all p< 0.05) (Figure 1).There were disciplinary differences in the relative importance of clinical variables to treatment decisions: more rheumatologists than pulmonologists rated as “very important” the extrapulmonary status of a patient’s SARD (51.1% vs. 35.0%) and the specific autoantibody (26.7% vs. 19.2%), whereas more pulmonologists rated as “very important” the radiographic pattern of ILD on high-resolution computed tomography (60.0% vs. 39.9%) and the presence of fibrosis (64.7% vs. 46.6%).Specialists also identified distinct scopes of decision-making responsibility and reported attending to disparate areas of healthcare maintenance. Rheumatologists were significantly more likely to screen for and treat osteoporosis, perform reproductive health counseling and ensure up-to-date cancer screening, whereas pulmonologists were more likely to screen for pulmonary hypertension and provide treatment for GERD, smoking cessation and PCP prophylaxis (all p< 0.05) (Table 2).
Conclusion: This national physician survey study suggests distinct specialty approaches to SARD-ILD management, and highlights opportunities to leverage complementary disciplinary expertise as part of a co-management framework.
To cite this abstract in AMA style:
Braverman G, Aronson K, Thomas C, Spiera R. Management of Interstitial Lung Disease in People with Systemic Autoimmune Rheumatic Diseases: A Comparison of Rheumatologist and Pulmonologist Perspectives [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/management-of-interstitial-lung-disease-in-people-with-systemic-autoimmune-rheumatic-diseases-a-comparison-of-rheumatologist-and-pulmonologist-perspectives/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/management-of-interstitial-lung-disease-in-people-with-systemic-autoimmune-rheumatic-diseases-a-comparison-of-rheumatologist-and-pulmonologist-perspectives/

.jpg)
.jpg)