Session Information
Date: Tuesday, October 28, 2025
Title: (2015–2051) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Aseptic abscess syndrome (AAS) is an inflammatory condition of unknown etiology, characterized by the formation of sterile neutrophilic abscesses that frequently respond to immunosuppressive therapy. We conducted a systematic review of all published AAS cases to describe its manifestations and outcomes.
Methods: This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (PROSPERO No. CRD42025641038). We searched PubMed/MEDLINE from inception through January 2025 using the terms “aseptic” and “abscess” or “abscesses” (Figure 1). Case reports and case series providing individual-level data were eligible for inclusion.
Results: A total of 73 studies describing 104 patients were included (54% female; median age: 32.5 years). The most frequently associated conditions were Crohn’s disease (n = 34, 33%), ulcerative colitis (n = 21, 20%), and Sweet’s syndrome (n = 8, 8%), which preceded the diagnosis of AAS in 50% of cases (Table 1). Common presenting symptoms included fever (n = 69, 66%), abdominal pain (n = 38, 37%), weight loss (n = 27, 26%), and pyoderma gangrenosum (n = 20, 19%).The spleen was the most frequent site of abscess development (n = 71, 68%), followed by the liver (n = 38, 37%), skin (n = 38, 37%), and lymph nodes (n = 33, 32%). The median number of organs involved was 2 (IQR: 2–3), with 49 (47%) patients having abscesses in three or more organs. Among those with available data, the median duration of symptoms before diagnosis was 2.3 months (IQR: 0.8–12).Most patients received corticosteroids (n = 93, 89%), with abscess resolution reported in 59 of 64 (92%) cases with available outcome data. Additional therapies included DMARDs (n = 47, 45%) and biologics (n = 29, 28%). Among the 74 patients with available data, antibiotics were administered in 42 (57%), for a median duration of 14 days (IQR: 7–26.5).Among 95 patients with follow-up data, 53 (56%) experienced at least one relapse. The median number of relapses was 1 (IQR: 0–2), with the first relapse occurring at a median of 3 months (IQR: 1–12). Relapses were more frequent among patients with splenic abscesses (64% vs. 35%, p = 0.011), lymph node involvement (71% vs. 48%, p = 0.038), and in those with abscesses affecting ≥3 organs (69% vs. 43%, p = 0.010). Notably, among 28 patients who underwent splenectomy, 20 (71%) experienced a relapse despite the procedure. Logistic regression demonstrated that the odds of relapse increased by 70% with each additional organ involved (OR = 1.70, 95% CI: 1.16–2.48, p = 0.007), and nearly tripled among patients with involvement of ≥3 organs (OR = 2.97, 95% CI: 1.28–6.89, p = 0.011). No deaths were reported.
Conclusion: AAS is often associated with underlying inflammatory disorders, particularly inflammatory bowel disease. Fever and splenic abscess are the most common manifestations. Despite high initial response rates to immunosuppressive therapy, relapses are common, particularly in patients with splenic, lymph node involvement, or multi-organ disease, while splenectomy does not appear to prevent recurrence. These findings may inform risk stratification and follow-up strategies in patients with multisystem disease.
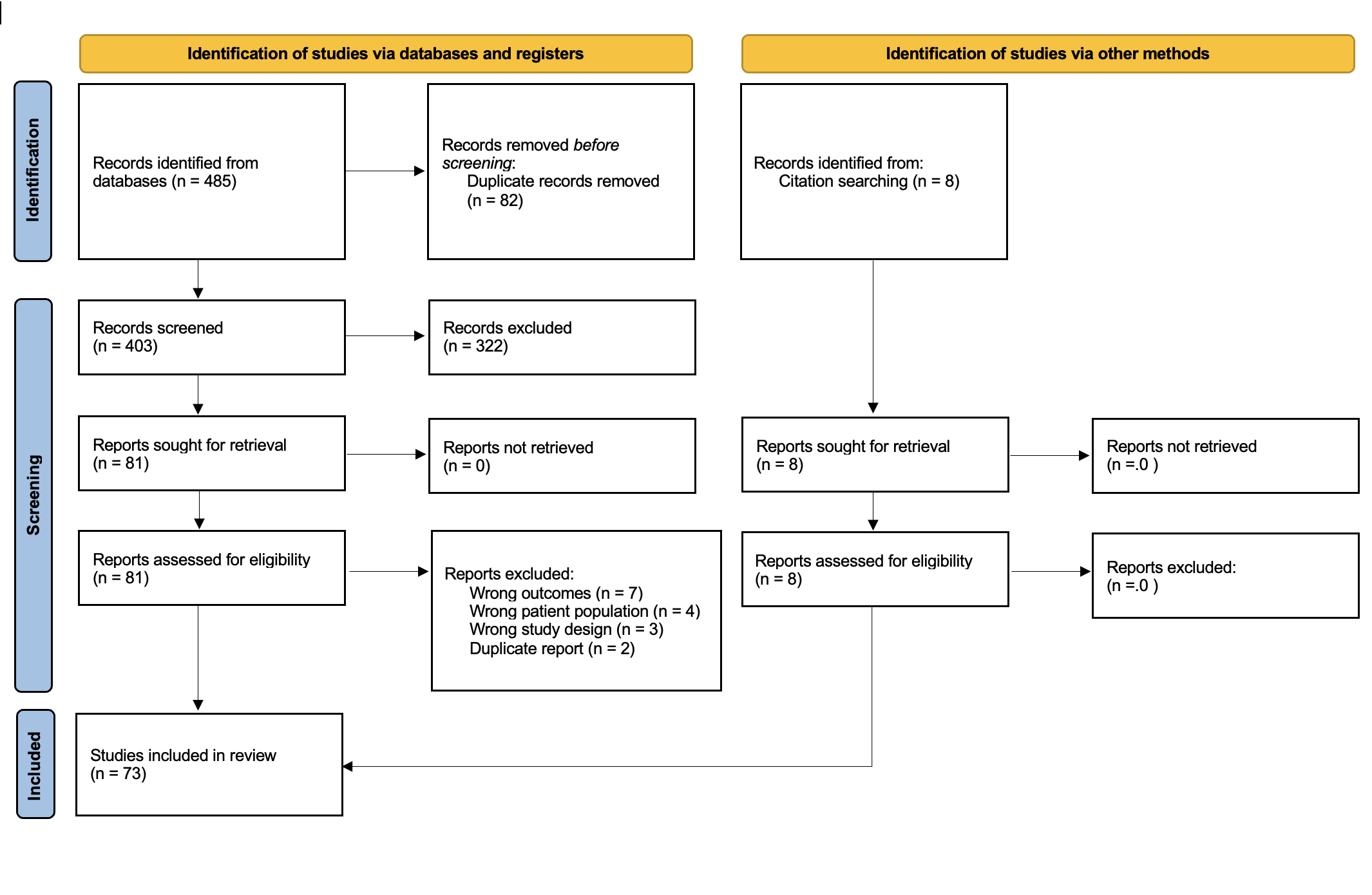 Table 1. Summary of patient characteristics, management, and outcomes.
Table 1. Summary of patient characteristics, management, and outcomes.
.jpg) Figure 1. The PRISMA flow diagram for the systematic review
Figure 1. The PRISMA flow diagram for the systematic review
To cite this abstract in AMA style:
Papachristodoulou E, Kakoullis L, Chopra R, Derk C, Parperis K. Clinical Features and Treatment Outcomes in Aseptic Abscess Syndrome: A Systematic Review of 104 Cases [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clinical-features-and-treatment-outcomes-in-aseptic-abscess-syndrome-a-systematic-review-of-104-cases/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-features-and-treatment-outcomes-in-aseptic-abscess-syndrome-a-systematic-review-of-104-cases/
