Session Information
Date: Tuesday, October 28, 2025
Title: (1972–1989) Measures & Measurement of Healthcare Quality Poster II
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Near-Infrared Spectroscopy combined with Vascular Occlusion Test (NIRS-VOT) is a non-invasive diagnostic method for assessing microvascular function. However, its diagnostic accuracy is often limited by inter-individual variability, particularly anatomical differences in vascular structure, such as brachial artery diameter (BAD). Since BAD significantly influences blood flow and may affect NIRS-VOT readings, we propose incorporating BAD as a reference parameter to standardize NIRS-VOT results and improve diagnostic reliability. This approach is particularly relevant in diseases like Antiphospholipid Syndrome (APS), a rare autoimmune disorder characterized by vascular dysfunction.
Methods: We applied this combined method to a cohort of 10 healthy controls (HCs) and 9 patients with APS. Brachial artery diameter was measured using ultrasound imaging, and NIRS-VOT was performed to assess tissue oxygen saturation (StO₂) parameters during vascular occlusion and reperfusion. We conducted correlation analyses to evaluate the relationship between BAD and NIRS-VOT parameters and performed logistic regression to examine whether including BAD improved classification between HCs and APS patients. Multiple statistical analyses were used to identify independent predictors of key NIRS-VOT outcomes.
Results: Our results indicate that incorporating BAD into NIRS-VOT significantly improves interpretation of hemodynamic parameters. In HCs, strong correlations were observed between BAD and NIRS-derived parameters (e.g., r = 0.95, p < 0.01), while correlations in APS patients were notably weaker, suggesting greater variability in vascular response. Both BAD and APS status emerged as significant independent predictors of key NIRS-VOT metrics. Logistic regression analysis showed that the inclusion of BAD improved classification accuracy—by at least 7.14% for baseline and minimum StO₂, and by up to 28.57% for maximum StO₂. Without BAD, the highest classification accuracy for maximum StO₂ was 78.57%, whereas including BAD increased it to 92.86%.
Conclusion: This study demonstrates the feasibility and utility of combining NIRS-VOT with ultrasound-derived BAD measurements for assessing microvascular function. To our knowledge, this is the first study to explore the interplay between conduit artery structure and NIRS-based functional assessments in this way. The integration of BAD into NIRS-VOT significantly enhances diagnostic accuracy, reduces inter-individual variability, and offers a more robust framework for evaluating vascular health. This approach shows promise not only for identifying vascular dysfunction in rare conditions such as APS but may also be applicable to other conduit arteries like the femoral artery, broadening the method’s potential clinical applications.
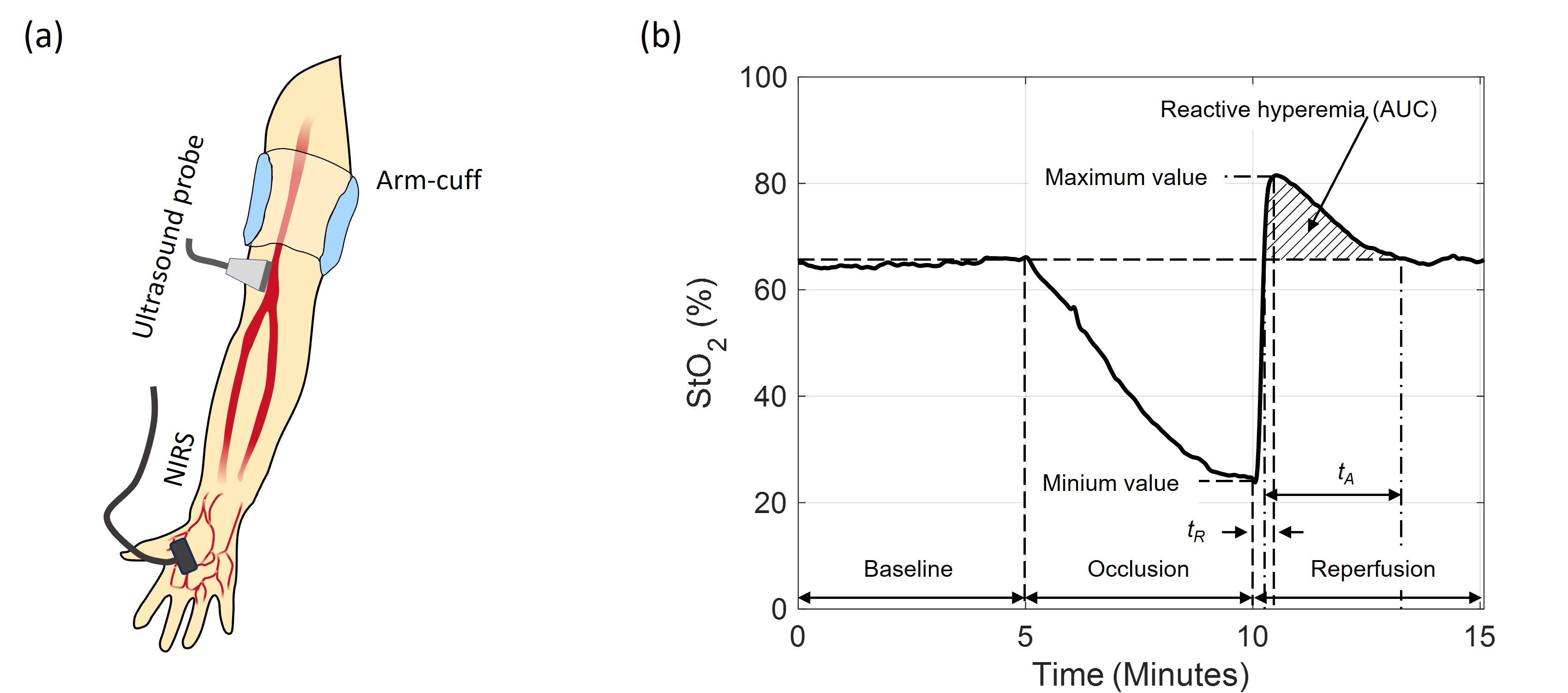 Figure 1. (a) Experimental setup combining a linear ultrasound probe on the upper arm to measure brachial artery diameter and a NIRS probe on the thenar for vascular occlusion testing (VOT). (b) Schematic of NIRS-derived tissue oxygen saturation (StO2) during VOT, including Baseline, Occlusion, and Reperfusion phases. Key parameters analyzed: baseline, minimum, maximum, resaturation time (tR), area under the curve (AUC), and hyperemic recovery time (tA).
Figure 1. (a) Experimental setup combining a linear ultrasound probe on the upper arm to measure brachial artery diameter and a NIRS probe on the thenar for vascular occlusion testing (VOT). (b) Schematic of NIRS-derived tissue oxygen saturation (StO2) during VOT, including Baseline, Occlusion, and Reperfusion phases. Key parameters analyzed: baseline, minimum, maximum, resaturation time (tR), area under the curve (AUC), and hyperemic recovery time (tA).
To cite this abstract in AMA style:
Park S, Mathew J, Osgood S, Gomez C, Leifer E, Sevim E, Kanthi Y. Advancing Vascular Assessment: Combining NIRS-VOT and Ultrasound-Based Brachial Artery Diameter for Improved Diagnostics in Healthy Controls and APS [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/advancing-vascular-assessment-combining-nirs-vot-and-ultrasound-based-brachial-artery-diameter-for-improved-diagnostics-in-healthy-controls-and-aps/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/advancing-vascular-assessment-combining-nirs-vot-and-ultrasound-based-brachial-artery-diameter-for-improved-diagnostics-in-healthy-controls-and-aps/
