Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Enteropathic spondyloarthritis (eSpA) is a subtype of SpA associated with inflammatory bowel disease (IBD). Sacroiliac joints (SIJs) involvement is common in eSpA but often clinically silent, contributing to diagnostic delay. Magnetic resonance imaging (MRI) enables detection of early inflammatory and structural changes, yet lesion patterns specific to eSpA insufficiently characterized. This study aimed to assess active and chronic inflammatory lesions on SIJ MRI.
Methods: We included 107 patients: 46 with IBD and 51 with axSpA with suspected eSpA, plus 10 with previously established eSpA. All underwent SIJ MRI; patients with MRI-confirmed sacroiliitis also underwent SIJs radiographs, scored using Bennett’s criteria (stage ≥2 sacroiliitis defined as positive for uni/bilateral involvement). MRI was assessed using the SPARCC scoring system for both active and structural lesions. The distribution of defined lesions were examined in four quadrants (scores ranging from 0-2 per quadrant on each sides of SIJ, expressed as mean (±SD)) and across slices. Two experienced readers, blinded to clinical data, independently scored all images; averaged scores were used. Cohen’s kappa showed high inter-reader reliability (BME: 0.8; fat metaplasia: 0.83; erosions: 0.88; backfill: 0.65; ankylosis: 0.84).
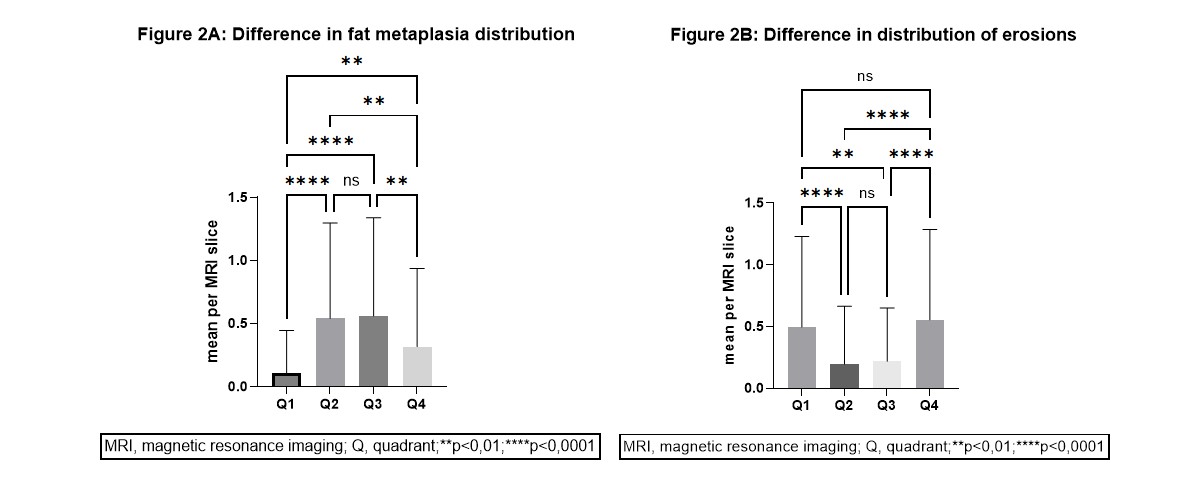
Results: Among 97 evaluated patients, 26 (27%) met classification criteria for eSpA. Including the 10 pre-diagnosed patients, 36 were analyzed: 20 (56%) had radiographic axSpA, 11 (31%) had non-radiographic axSpA, and 5 (14%) had unknown status due to missing x-ray data. Radiographic sacroiliitis was bilateral in 18 (58%), unilateral in 8 (26%), and absent (stage < 2) in 5 (16%). MRI revealed distinct quadrant-level lesion patterns. Bone marrow edema (BME) was significantly more prevalent in Q4 compared to Q1 and Q2 (0.5 (± 0.6) vs. 0.2 (±0.5) and 0.3 (±0.6), p< 0.0001 and < 0.0001, respectively) and in Q3 compared to Q1 (0.4 (±0.7) vs. 0.2 (±0.5), p=0.0023), with no significant difference between Q4 and Q3 (Figure 1). Fat metaplasia was significantly more frequent in Q2 and Q3 compared to Q1 and Q4 (0.5 (±0.8) and 0.6 (±0.8) vs. 0.1 (±0.3) and 0.3 (±0.6) SPARCC SIJ structural score, p< 0.0001, p=0.0051, p< 0.0001, p=0.0033, respectively) and between Q1 and Q4 (0.1 (±0.3) and 0.3 (±0.6), p=0.0043) (Figure 2). Erosions were significantly more frequent in Q1 and Q4 compared to Q2 and Q3 (0.5 (±0.7) and 0.6 (±0.7) vs. 0.2 (±0.5) and 0.2 (±0.4), p< 0.0001, p=0.0030, p< 0.0001, p< 0.0001, respectively) (Figure 2). No significant differences were observed in lesion distribution across MRI slices. Patients with Crohn’s disease exhibited significantly more erosions than those with ulcerative colitis (8.5 (±6.2) vs. 3.5 (±4.1), p=0.0286) (Figure 3).
Conclusion: Most patients with eSpA demonstrate bilateral SIJ involvement on radiographs. MRI revealed distinct patterns of inflammatory and structural lesions, with quadrant-specific predilections for BME, fat metaplasia, and erosions. Crohn’s disease was associated with a higher burden of erosive changes compared to ulcerative colitis, suggesting phenotypic heterogeneity in musculoskeletal manifestations of eSpA.Supported by: SVV 260 683, GAUK 310525
 Difference in bone marrow edema distribution
Difference in bone marrow edema distribution
.jpg) Difference in fat metaplasia distribution, Difference in distribution of erosions
Difference in fat metaplasia distribution, Difference in distribution of erosions
.jpg) Presence of erosions in patients with SpA/IBD: ulcerative colitis vs. Crohn disease
Presence of erosions in patients with SpA/IBD: ulcerative colitis vs. Crohn disease
To cite this abstract in AMA style:
Bodnárová M, Ondrejčáková L, Grega T, Šenolt L, Pavelka K, Bubová K. Imaging findings in patients with enteropathic spondyloarthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/imaging-findings-in-patients-with-enteropathic-spondyloarthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/imaging-findings-in-patients-with-enteropathic-spondyloarthritis/
