Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: In the last decade, rheumatologists have employed musculoskeletal Ultrasound (MSUS) as a highly sensitive and accurate clinical assessment tool at the bedside. By integrating complementary specialties, interdisciplinary clinics aim to enhance patient outcomes. Here, we introduce a novel Rheumatology and Hand Surgery interdisciplinary clinic and examine the patient outcomes when MSUS is used for assessment of active joint disease.
Methods: We conducted a retrospective chart review of 218 patients seen at a Rheumatology-Plastic Surgery interdisciplinary hand clinic from January 2018 to May 2024. Demographics data, use of MSUS diagnostically, frequency of modifying disease-modifying antirheumatic drugs (DMARDSs) escalation/surgery, and out data were compared and analysed.
Results: With MSUS implementation, subclinical synovitis was detected in 31% of patients (whereas clinical synovitis was only detected in 12% of patients on physical exam only). As patients with active synovitis are recommended escalation of DMARDs rather than surgical management, there was a 25.8% absolute reduction in surgery recommendation (from 60% to 34%), and a 26.2% absolute increase in DMARD escalation recommendation (from 5% to 31%).
Conclusion: The use of MSUS significantly improves the detection of active inflammatory arthritis in referred patients, resulting in increased DMARD escalation and decreased surgery recommendations. These data suggest that it may be beneficial to incorporate MSUS into standard care. The use of MSUS may aid in identifying patients with active disease, such that these patients may be medically optimized with DMARDSs and potentially avoid surgical intervention.
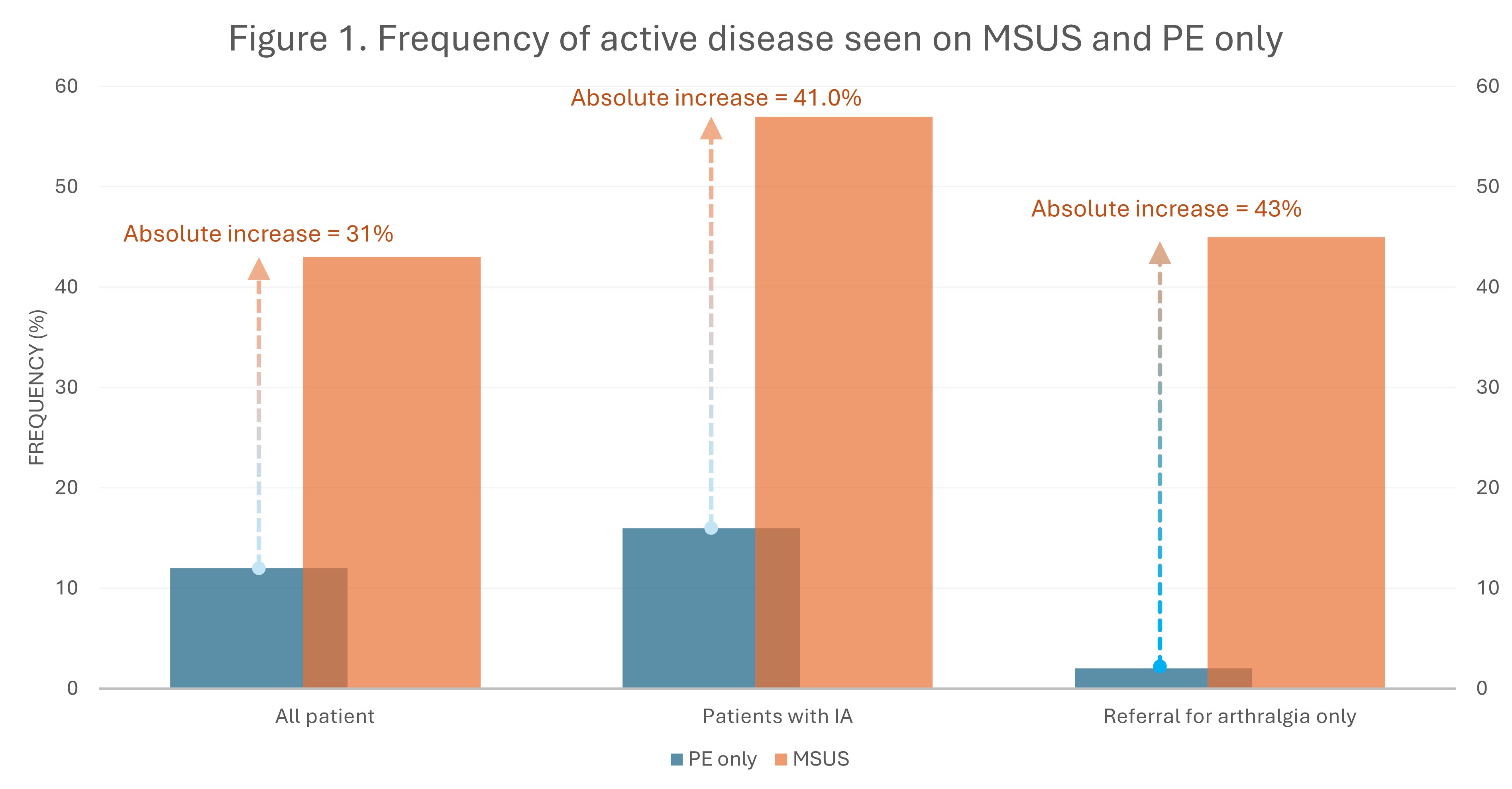 Figure 1 shows how commonly active inflammatory hand disease was found on assessment with physical exam alone as compared to with MSUS. It shows the comparison for all patients who attended the clinic, as well as two subgroups: patients referred with confirmed inflammatory arthritis and patients referred for pain as their main concern.
Figure 1 shows how commonly active inflammatory hand disease was found on assessment with physical exam alone as compared to with MSUS. It shows the comparison for all patients who attended the clinic, as well as two subgroups: patients referred with confirmed inflammatory arthritis and patients referred for pain as their main concern.
.jpg) Figure 2 shows how commonly surgery was recommended with physical exam alone as compared to with MSUS. It shows the comparison for all patients who attended the clinic, as well as two subgroups: patients referred with confirmed inflammatory arthritis and patients referred for pain as their main concern.
Figure 2 shows how commonly surgery was recommended with physical exam alone as compared to with MSUS. It shows the comparison for all patients who attended the clinic, as well as two subgroups: patients referred with confirmed inflammatory arthritis and patients referred for pain as their main concern.
.jpg) Figure 3 shows how commonly DMARD escalation was recommended with physical exam alone as compared to with MSUS. It shows the comparison for all patients who attended the clinic, as well as two subgroups: patients referred with confirmed inflammatory arthritis and patients referred for pain as their main concern.
Figure 3 shows how commonly DMARD escalation was recommended with physical exam alone as compared to with MSUS. It shows the comparison for all patients who attended the clinic, as well as two subgroups: patients referred with confirmed inflammatory arthritis and patients referred for pain as their main concern.
To cite this abstract in AMA style:
pye A, Chan S, Xu G, Bardi M. Optimizing Patient Outcomes: The Experience of a Multidisciplinary Rheumatology and Hand Surgery Clinic with Point-of-Care Musculoskeletal Ultrasound Integration [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/optimizing-patient-outcomes-the-experience-of-a-multidisciplinary-rheumatology-and-hand-surgery-clinic-with-point-of-care-musculoskeletal-ultrasound-integration/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/optimizing-patient-outcomes-the-experience-of-a-multidisciplinary-rheumatology-and-hand-surgery-clinic-with-point-of-care-musculoskeletal-ultrasound-integration/
