Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) are vulnerable to infections due to both underlying immune dysfunction and the use of immunosuppressive therapies. Hence, it was assumed that patients with SLE would experience disproportionately poor outcomes during the COVID-19 pandemic. We aimed to evaluate changes in SLE mortality in relation to the COVID-19 pandemic: before (2018–2019), during (2020–2022), and after (2023); and to assess whether these trends differed from all-cause mortality.
Methods: We retrieved mortality data for SLE from the CDC national mortality database, and calculated age-standardized mortality rates (ASMRs) per million population with 95% confidence intervals (CI), overall and by race/ethnicity, age group (≤44, 45–64, ≥65 years), sex, and U.S. census region (Northeast, Midwest, South, West) across three time periods: pre-pandemic (2018–2019), during the pandemic (2020–2022), and post-pandemic (2023). We repeated these analyses for all-cause deaths other than SLE (non-SLE). We then computed ratios of SLE ASMR to non-SLE ASMR to contextualize lupus mortality within overall general population mortality trends. We performed percent change calculations between the three periods.
Results: SLE-ASMR increased from 6.1 per million (95% CI, 5.9–6.3) pre-pandemic to 7.1 (95% CI: 6.9–7.2) during the pandemic, before declining to 5.8 (95% CI: 5.5–6.0) post-pandemic. Non-SLE ASMR followed a similar trend, however, non-SLE ASMR remained significantly elevated post-pandemic compared to pre-pandemic levels. Consequently, the ratio of SLE-ASMR to non-SLE-ASMR continued to decline from the pre-pandemic to pandemic years (by 0.83%) and from the pandemic to post-pandemic years (by 8.71%). This trend was seen in all subpopulations by race/ethnicity, age, sex, and geographic region, except in individuals aged ≥65 years and those living in the South census region of the U.S. that experienced increases in the ratio.
Conclusion: This nationwide analysis shows that SLE mortality did not increase disproportionately during the COVID-19 pandemic, and that it declined more than the all-cause mortality after the pandemic. However, certain subgroups including older individuals and people in the South, experienced relatively higher SLE mortality during the pandemic. Further analyses of reasons underlying these trends, including the precise identification of subpopulations in the South that had the highest SLE mortality during the pandemic, would have implications for managing these at-risk subpopulations during future viral outbreaks and medical emergencies.
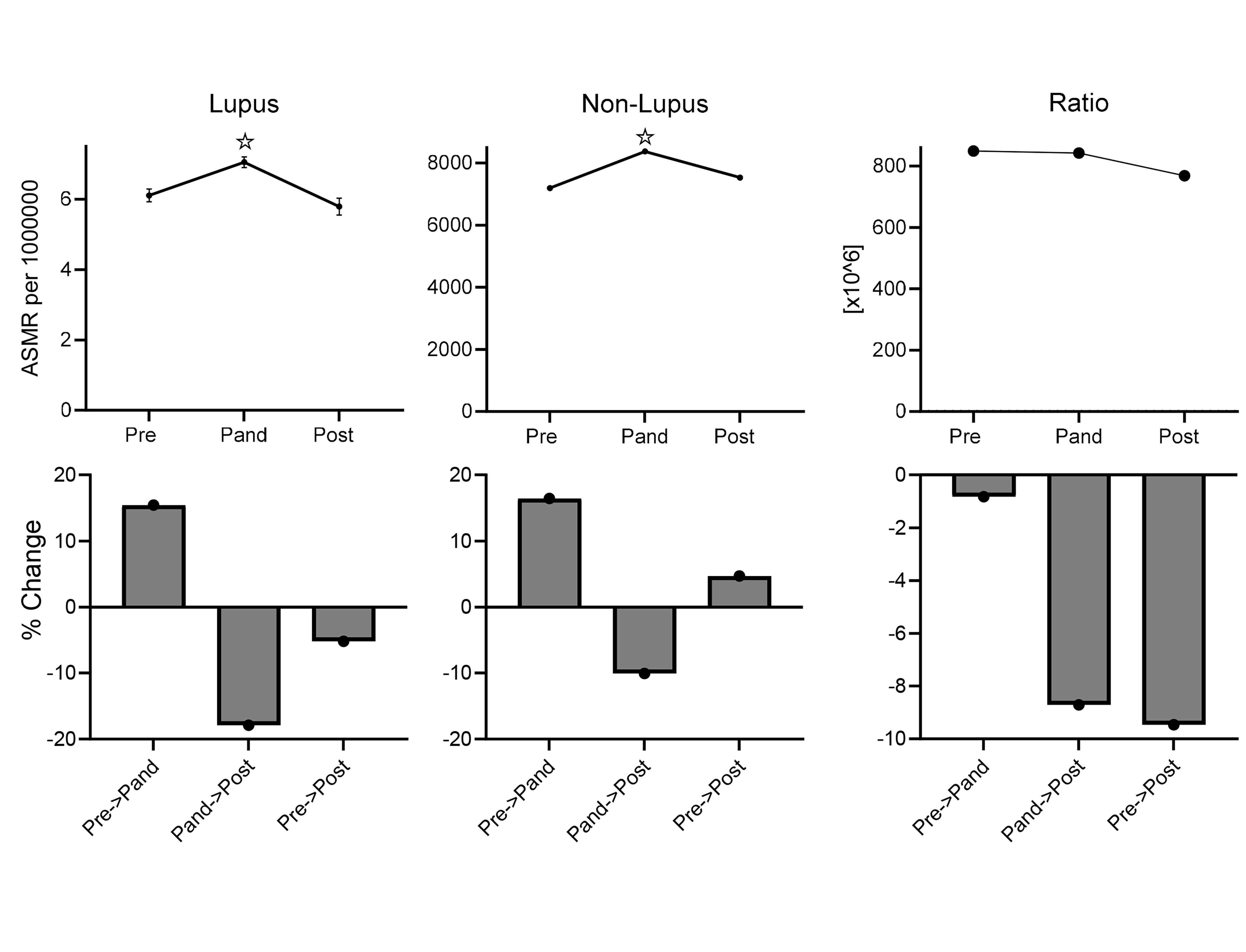 Age standardized mortality rates for SLE before (2018-2019), during (2020-2022), and after (2023) the COVID-19 pandemic.
Age standardized mortality rates for SLE before (2018-2019), during (2020-2022), and after (2023) the COVID-19 pandemic.
To cite this abstract in AMA style:
Hernandez L, Singh R. Changes in SLE Mortality During and After the COVID-19 Pandemic [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/changes-in-sle-mortality-during-and-after-the-covid-19-pandemic/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/changes-in-sle-mortality-during-and-after-the-covid-19-pandemic/
