Session Information
Date: Monday, October 27, 2025
Title: Abstracts: ARP I: Multidimensional Influences on Health in SLE (1686–1691)
Session Type: Abstract Session
Session Time: 3:30PM-3:45PM
Background/Purpose: This study aimed to examine the impact of psychological distress—specifically stress, anxiety, and depression—on fatigue in rheumatology patients, and explored how this relationship is moderated by trauma exposure and resilience. Understanding these dynamics is essential for developing holistic psychosocial interventions for individuals with chronic autoimmune disorders.
Methods: A quantitative, non-experimental comparative design with a between-groups approach was employed using convenience sampling. The sample comprised 132 participants recruited from the outpatient departments of KIMS Hospitals, Secunderabad, and HRC Hospital, Begumpet. Participants included 95 females and 37 males, aged 19 to 78 years (M = 42.7), diagnosed with Rheumatoid Arthritis (n = 36), Spondyloarthritis (n = 32), Psoriatic Arthritis (n = 26), or Systemic Lupus Erythematosus (n = 38). A General Information Schedule was used to collect demographic data. Disease activity was assessed using DAS-28, ASDAS, cDAPSA, or SLEDAI as appropriate. Fatigue was measured using the FACIT-Fatigue Scale (Version 4). Depression, Anxiety, and Stress were assessed using the DASS-42. Trauma exposure was measured using the Brief Trauma Questionnaire (BTQ), which included items on emotional abuse, familial illness, and pregnancy-related issues. Resilience was assessed using the abbreviated Nicholson McBride Resilience Questionnaire. Data were analyzed using JAMOVI. Descriptive statistics were calculated, and normality tested with the Shapiro-Wilk test. Inferential analyses included the Mann-Whitney U test, Kruskal-Wallis test, Spearman’s correlation matrix, and path analysis using the SEMLj module.
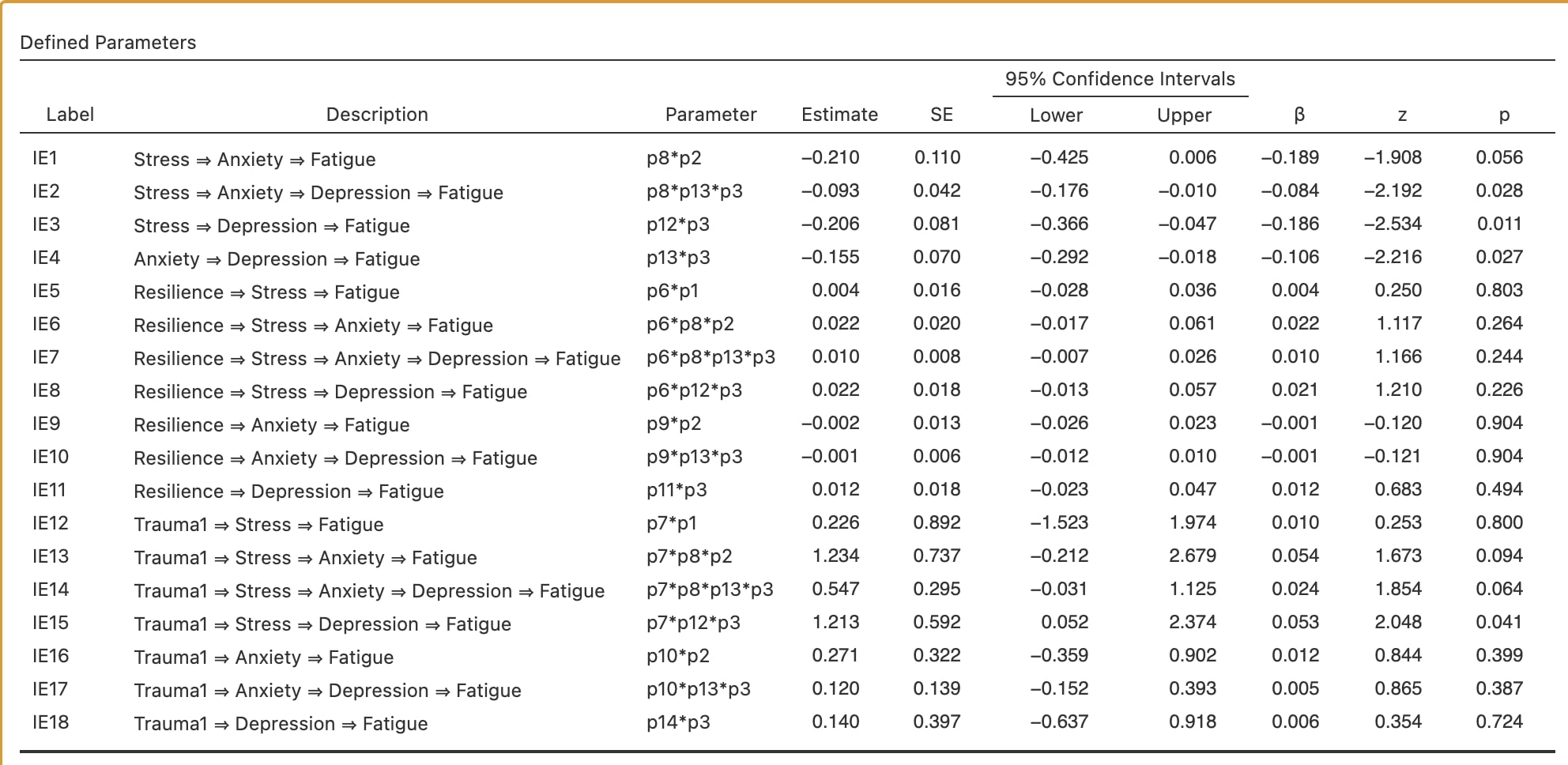
Results: While no significant group differences were found, Spearman’s correlation revealed that higher psychological distress is linked to greater fatigue, while resilience showed a protective effect, implying complex, non-linear relationships, supporting the use of structural equation modeling to clarify how resilience may buffer the impact of trauma-related distress on fatigue. The path model demonstrated excellent fit (CFI = 1.000; RMSEA = 0.000). Depression was the strongest direct predictor of fatigue (β = -0.34, p = 0.006); anxiety had a marginal effect; stress influenced fatigue only indirectly. Resilience did not significantly mediate or moderate these paths, potentially due to the small, non-normally distributed sample, which may have limited power to detect subtle effects.
Conclusion: The findings underscore the critical role of psychological factors—particularly stress, anxiety, and depression—in the experience of fatigue among patients with rheumatological conditions. Trauma exerts an indirect effect, while resilience showed no significant buffering, possibly due to sample size and distribution limitations. Results support the need for integrated care. Interventions could be two-pronged: one path reducing psychological distress, the other bolstering resilience, thereby addressing fatigue from two converging angles. Future research will expand the sample and test the effectiveness of such interventions.
 Spearman’s Correlation Matrix among the variables.
Spearman’s Correlation Matrix among the variables.
.jpg) Mediation Analysis (indirect effects) of the hypothesied Path Model
Mediation Analysis (indirect effects) of the hypothesied Path Model
.jpg) The Hypothesized Path Model showing the direct and indirect effects of the studied variables
The Hypothesized Path Model showing the direct and indirect effects of the studied variables
To cite this abstract in AMA style:
Veeravalli A, gajjala S, Veeravalli S. Impact of Stress, Anxiety, and Depression on Fatigue as moderated by Resilience and Exposure to Trauma in Rheumatology Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-stress-anxiety-and-depression-on-fatigue-as-moderated-by-resilience-and-exposure-to-trauma-in-rheumatology-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-stress-anxiety-and-depression-on-fatigue-as-moderated-by-resilience-and-exposure-to-trauma-in-rheumatology-patients/
