Session Information
Date: Monday, October 27, 2025
Title: (1517–1552) Systemic Lupus Erythematosus – Treatment Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a chronic multisystem autoimmune disease associated with increased morbidity and mortality, particularly due to cardiovascular complications. Atherosclerotic cardiovascular disease (ASCVD) has emerged as one of the leading causes of death in young patients with SLE. This elevated cardiovascular risk cannot be fully explained by traditional risk factors alone, suggesting that disease-specific mechanisms, including chronic inflammation, immune dysregulation, and treatment-related factors, play a pivotal role. We aimed to evaluate the impact of prednisone in patients with SLE on lipid profile and the risk of subclinical atherosclerosis.
Methods: A cross-sectional, comparative, and analytical case-control study was conducted. Eighty patients, older than 18 years, who met the classification criteria for SLE according to ACR/EULAR 2019 criteria guidelines were enrolled.Carotid ultrasound was accomplished in 34 patients, and the presence of plaque was recorded, defined as wall thickening greater than 50%, or a focal region with a measurement greater than 1.5 mm that protrudes into the lumen. CIMT was also registered. The descriptive analysis was done with frequencies (%), mean (± SD), median (q25-q75), and comparisons with Chi square and Student’s T, accordingly. We considered p < 0.05 as statistically significant. Statistical analysis was performed using SPSS version 25 (IBM, New York, USA).
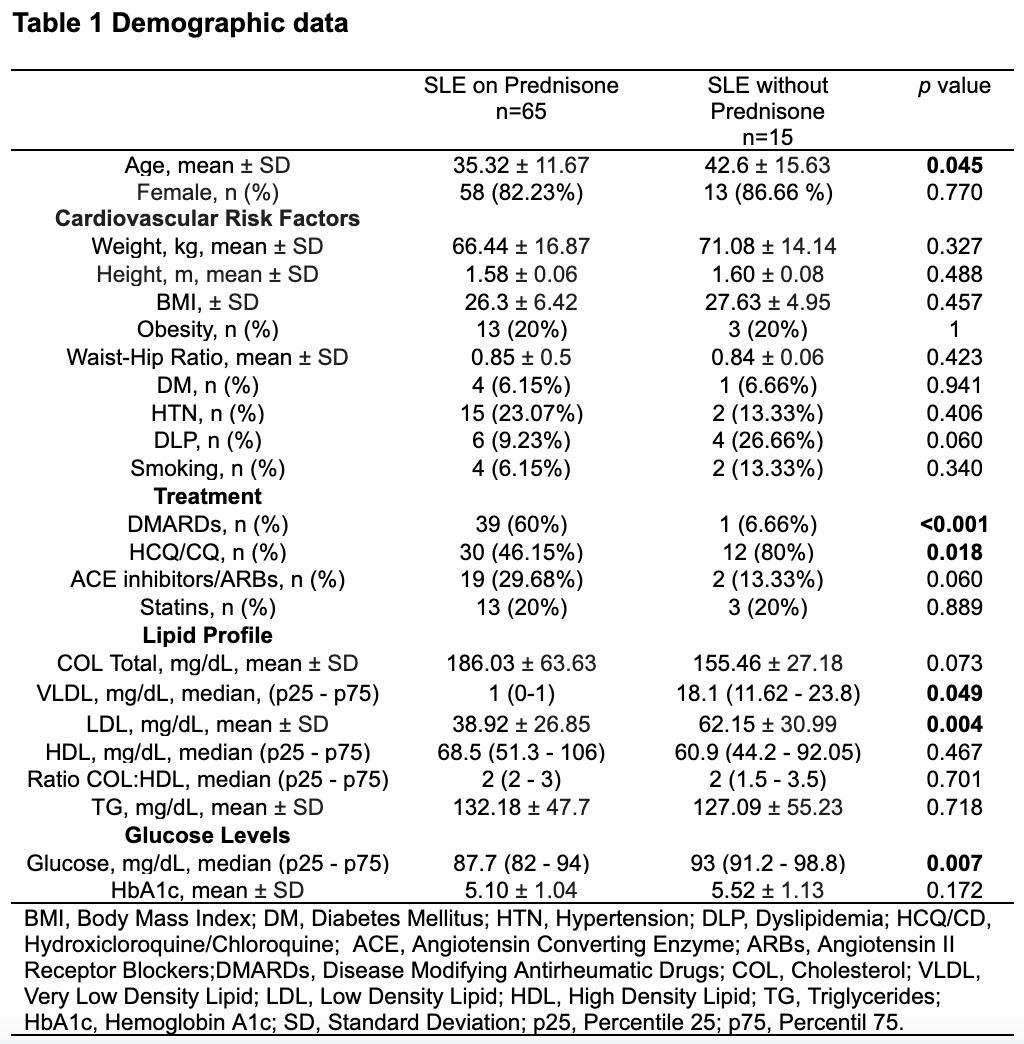
Results: In this cohort study of patients with SLE, those receiving prednisone were significantly younger (35.32 ± 11.67 vs. 42.6 ± 15.63 years, p = 0.045) and more frequently treated with DMARDs (39 [60%] vs 1 [6.66%] p < 0.001), while hydroxychloroquine/chloroquine use was higher in the non-prednisone group (p = 0.018). There were no significant differences in traditional cardiovascular risk factors like obesity, diabetes, hypertension, or smoking. Despite the known adverse metabolic effects of corticosteroids, patients not on prednisone had significantly higher levels of VLDL (p = 0.049), LDL cholesterol (p = 0.004), and fasting glucose (p = 0.007), suggesting a paradoxical trend toward a worse metabolic profile in those without steroids (Table 1). In a subset of 34 patients who underwent carotid ultrasound, right carotid intima-media thickness (CIMT) was also significantly greater in the non-prednisone group (0.43 ± 0.069 vs 0.52 ± 0.17 p = 0.046), indicating more subclinical atherosclerosis (table 2).
Conclusion: This study suggests that in patients with SLE, prednisone use despite its known metabolic side effects, was paradoxically associated with a more favorable lipid and glucose profile, as well as lower carotid intima-media thickness, compared to those not on prednisone. There were no significant differences in traditional cardiovascular risk factors or carotid plaque presence. These findings indicate that the anti-inflammatory effects of prednisone may, in certain contexts, mitigate metabolic and vascular risks, potentially reducing subclinical atherosclerosis. However, further longitudinal studies are needed to better understand its long-term cardiovascular impact in SLE.
To cite this abstract in AMA style:
Garza-Gonzalez E, Garcia-Garcia F, Garza-Flores O, Polina-Lugo R, Lopez-Cantú L, Azpiri-Lopez J, Colunga-Pedraza I, Cardenas-de la Garza J, Galarza-Delgado D, Salcedo Almanza D. Influence of Prednisone use over cardiovascular risk in patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/influence-of-prednisone-use-over-cardiovascular-risk-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/influence-of-prednisone-use-over-cardiovascular-risk-in-patients-with-systemic-lupus-erythematosus/

.jpg)