Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Axial involvement is one of the key features of psoriatic arthritis (PsA) and is associated with increased disease burden. However, rates and predictors of structural damage progression in the spine in PsA are not well defined. This study aimed to explore associations between factors reflecting activity and severity across PsA domains and the development and progression of structural damage in the spine in a large longitudinal cohort.
Methods: We analyzed patients from a prospective longitudinal PsA cohort. Axial damage was assessed using two outcomes: (1) syndesmophyte development (binary), and (2) modified Stoke Ankylosing Spondylitis Spine Score (mSASSS, continuous). Cox proportional hazards models were used for syndesmophyte development, and generalized estimating equation (GEE) models were used for mSASSS progression. Variables reflecting activity/severity included cDAPSA, swollen joint count (SJC), SPARCC enthesitis score, dactylitis, nail involvement, PASI, modified Steinbrocker score, radiographic sacroiliitis score (sum of grades on two sides; range 0-8), BASDAI, ESR, and CRP. Multivariable models were adjusted for potential confounders, including age, sex, PsA duration, BMI, smoking status, decade of observation, HLA-B*27, HLA-A*29 (known to be associated with a reduced risk of axial disease), radiographic sacroiliitis score (where appropriate), NSAID use, and biologic or targeted synthetic (b/ts) DMARD use. Lastly, we conducted sensitivity analyses stratified by observation period (pre-2000 vs. 2000 and beyond).
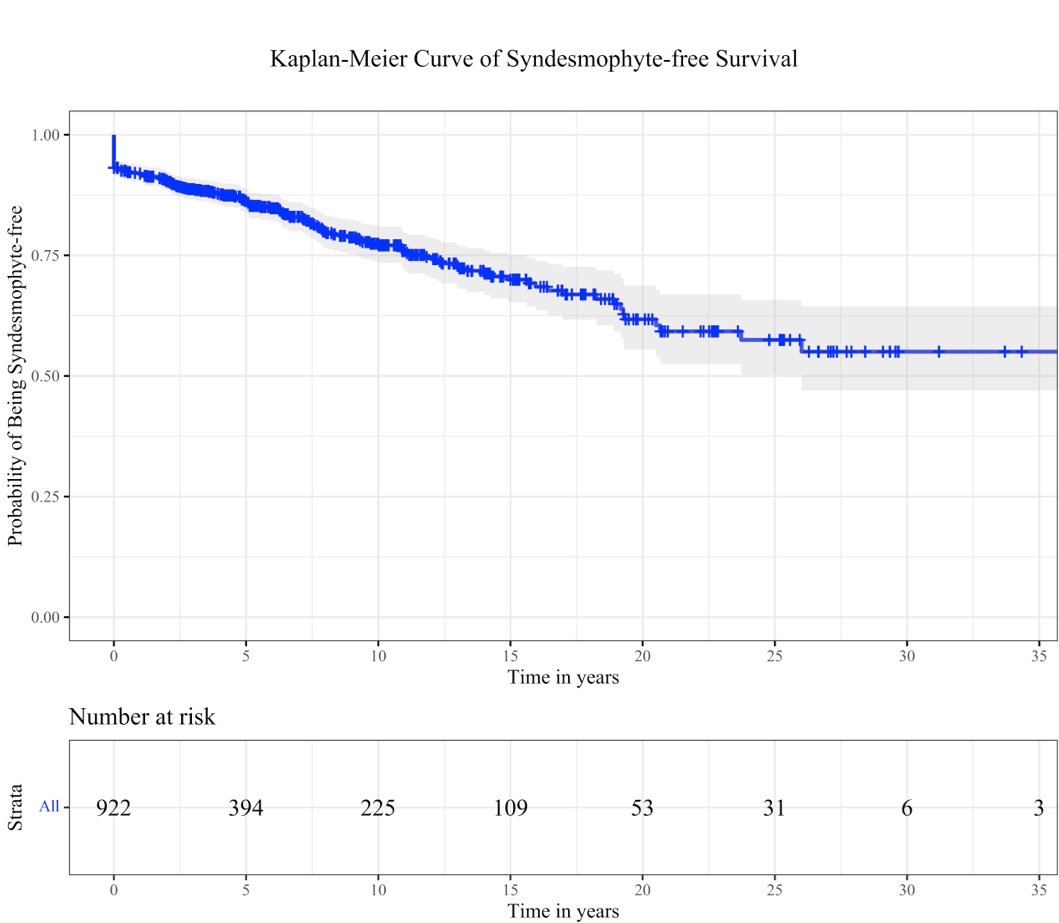
Results: The study included 1584 patients with PsA, with a median age of 45 years [IQR: 34.3–54.7]. At baseline (clinic entry), 218 patients (13.8%) had syndesmophytes. The median mSASSS was 0 [IQR: 0–0], while the mean (SD) was 1.6 (6.2). Over the study follow-up period, 166 of the 922 individuals (18.0%) without syndesmophytes at baseline who had repeat spine X-rays developed syndesmophytes, with a median time to development of 5.8 years [IQR: 2.4, 9.9].Figure 1 shows a Kaplan-Meier curve of syndesmophyte-free survival, with the results of the univariable models shown in Table 1. In multivariable Cox models (Figure 2A), higher ESR (HR 1.02, 95% CI 1.01–1.03) and radiographic sacroiliitis score (HR 1.19, 95% CI 1.07–1.32) were significantly associated with syndesmophyte development. In multivariable GEE models (Figure 2B), higher CRP (estimate 0.04, 95% CI 0.004–0.08) and sacroiliitis score (estimate 0.70, 95% CI 0.40–1.00) were associated with mSASSS progression. Sensitivity analyses confirmed consistent findings across observation periods.
Conclusion: Systemic inflammation, reflected by elevated ESR and CRP levels, was the strongest predictor of radiographic spinal progression in axial PsA. Radiographic sacroiliitis also showed an association with structural damage in the spine in PsA.
 Abbreviations: HR: Hazard Ratio, CI: Confidence Interval, PsA: Psoriatic Arthritis, BMI: Body Mass Index, SJC: Swollen Joint Count, cDAPSA: Composite Disease Activity Index for Psoriatic Arthritis, SPARCC: Spondyloarthritis Research Consortium of Canada, PASI: Psoriasis Area and Severity Index, BASDAI: Bath Ankylosing Spondylitis Disease Activity Index, ESR: Erythrocyte Sedimentation Rate, CRP: C-Reactive Protein, HLA: Human Leukocyte Antigen, NSAIDs: Non-Steroidal Anti-Inflammatory Drugs, DMARDs: Disease-Modifying Anti-Rheumatic Drugs.
Abbreviations: HR: Hazard Ratio, CI: Confidence Interval, PsA: Psoriatic Arthritis, BMI: Body Mass Index, SJC: Swollen Joint Count, cDAPSA: Composite Disease Activity Index for Psoriatic Arthritis, SPARCC: Spondyloarthritis Research Consortium of Canada, PASI: Psoriasis Area and Severity Index, BASDAI: Bath Ankylosing Spondylitis Disease Activity Index, ESR: Erythrocyte Sedimentation Rate, CRP: C-Reactive Protein, HLA: Human Leukocyte Antigen, NSAIDs: Non-Steroidal Anti-Inflammatory Drugs, DMARDs: Disease-Modifying Anti-Rheumatic Drugs.
*Sum of the two sides (0-8)
.jpg) Figure 1. Kaplan–Meier survival analysis depicting the probability of remaining syndesmophyte-free over time.
Figure 1. Kaplan–Meier survival analysis depicting the probability of remaining syndesmophyte-free over time.
.jpg) Figure 2. A: Multivariable Cox proportional hazards models identifying factors associated with syndesmophyte development in patients with psoriatic arthritis (PsA).
Figure 2. A: Multivariable Cox proportional hazards models identifying factors associated with syndesmophyte development in patients with psoriatic arthritis (PsA).
B: Multivariable generalized estimating equation (GEE) models identifying factors associated with mSASSS progression among PsA patients.
Abbreviations: HLA-B*27: Human Leukocyte Antigen B*27; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; ESR: Erythrocyte Sedimentation Rate; PASI: Psoriasis Area and Severity Index; CRP: C-Reactive Protein; SJC: Swollen Joint Count; cDAPSA: Clinical Disease Activity Index for Psoriatic Arthritis; DMARDs: Disease-Modifying Antirheumatic Drugs; SPARCC: Spondyloarthritis Research Consortium of Canada.
To cite this abstract in AMA style:
Kharouf F, Mehta P, Carrizo Abarza V, Gao S, Pereira D, Gladman D, Chandran V, Poddubnyy D. Structural Damage Progression in the Spine in Patients with Psoriatic Arthritis: Findings from a Longitudinal Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/structural-damage-progression-in-the-spine-in-patients-with-psoriatic-arthritis-findings-from-a-longitudinal-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/structural-damage-progression-in-the-spine-in-patients-with-psoriatic-arthritis-findings-from-a-longitudinal-cohort-study/
