Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is a severe complication of rheumatoid arthritis (RA), associated with increased morbidity and mortality. The pulmonary safety of biologic (bDMARDs) and targeted synthetic DMARDs (tsDMARDs) in RA-ILD remains unclear due to limited and heterogeneous data. The aim is to assess the impact of bDMARDs and tsDMARDs on interstitial lung disease in rheumatoid arthritis.
Methods: The SLR aimed to include all reports of controlled trials and observational studies of biological and targeted synthetic disease-modifying antirheumatic drugs (DMARDs) used in patients with a diagnosis of RA, defined as fulfilment of the 1987 ACR criteria or 2010 ACR/EULAR criteria. We searched PubMed and Cochrane databases for English articles published until 2025 using the keywords « interstitial lung disease AND “Arthritis, Rheumatoid”[Mesh]) AND “Arthritis, Rheumatoid/therapy”[Mesh] ». The MA was performed with Review Manager (RevMan v.5.4.1) software with the inverse variance method on FVC and DLCO parameters.
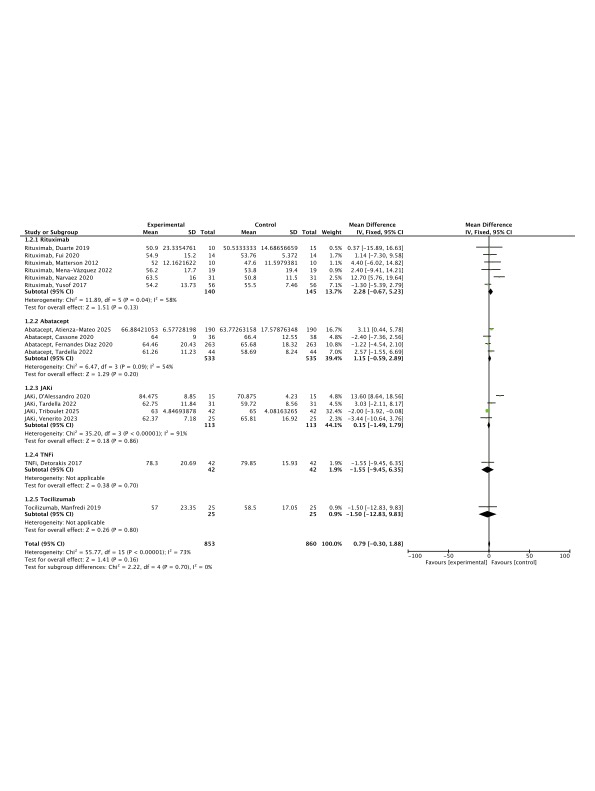
Results: Out of 861 abstracts screened, 15 observational studies were included, evaluating the effects of abatacept, rituximab, tocilizumab, TNF inhibitors (TNFi), and Janus kinase inhibitors (JAKi) on RA-ILD. These studies collectively involved 958 patients (mean age: 65 years; 57% female) with a mean disease duration of 115 months. Among the ILD patterns, usual interstitial pneumonia (UIP) accounted for 48% and non-specific interstitial pneumonia (NSIP) for 40%. Data on changes in DLCO and FVC were available from 6 studies on rituximab, 4 on abatacept, 4 on JAK inhibitors, 1 on TNFi, and 1 on tocilizumab.Analysis of FVC (%) variation before and after treatment revealed no significant overall change across all therapies (mean difference: -0.85%, 95% CI [-2.40, 0.71]; p=0.29). Rituximab was the only agent associated with a potential increase in mean FVC (+3.39%, 95% CI [-2.75, 9.53]), although this difference did not reach statistical significance (p=0.28). Similarly, DLCO values remained stable following treatment (mean difference: +0.79, 95% CI [-0.30, 1.88]; p=0.16). No statistically significant differences were observed between the individual treatment groups.
Conclusion: In conclusion, while bDMARDs and tsDMARDs show potential in stabilizing pulmonary function in RA-ILD, no significant differences were observed between treatments, highlighting the need for further research to clarify their impact on interstitial lung disease progression.
To cite this abstract in AMA style:
HILLIQUIN S, VISMARA E, BERLENGIERO V, AVOUAC J. Effect of bDMARDs and tsDMARDS on diffuse interstitial lung disease associated with rheumatoid arthritis: systematic review and meta-analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/effect-of-bdmards-and-tsdmards-on-diffuse-interstitial-lung-disease-associated-with-rheumatoid-arthritis-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-bdmards-and-tsdmards-on-diffuse-interstitial-lung-disease-associated-with-rheumatoid-arthritis-systematic-review-and-meta-analysis/

.jpg)