Session Information
Date: Monday, October 27, 2025
Title: (1221–1247) Pain in Rheumatic Disease Including Fibromyalgia Poster
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Over one third of older Americans experience chronic pain, accompanied by age-related increases in pain-related activity interference (i.e., pain burden). While pain extent (i.e., the number of reported pain sites) is often used as an indicator of this burden, extent tends to plateau or decline after midlife. Thus, it is unclear whether the same pain extent represents the same level of burden in oldest-old adults as it does in younger-old counterparts. Furthermore, there are different ways of assessing pain extent, some of which may better capture the impact of the chronic pain experience. We therefore estimated the prevalence and burden of several chronic pain definitions among older adults by age and sex.
Methods: We used data from a community-based sample of older adults from an ancillary study of the Framingham Heart Study/Omni1. We collected data on number and distribution of pain sites (articular, non-articular, and axial), pain duration, frequency, intensity, and interference with daily activities. We categorized participants with chronic pain (i.e., pain lasting ≥3 months) into 3 extent-based groups: 1) chronic widespread pain (WSP) as pain present above and below the waist, on the right and left sides of the body, and in the spine. 2) chronic multisite pain as pain occupying ≥3 body sites (and not meeting the WSP definition), and 3) chronic pain in 1-2 pain sites. We additionally characterized participants with bothersome or high-impact chronic pain (B-HICP) based upon high pain frequency, intensity, and interference from the Brief Pain Inventory. For each of the 4 pain categorizations, we compared their frequencies across age groups (52-70, 71-80, 81+ years) in a sex-stratified manner and assessed for linear trends. We also assessed mean pain interference from the Brief Pain Inventory for each of the extent-based categorizations across age groups in a sex-specific manner using linear regression. We did not do so for B-HICP because pain interference is included in its definition.
Results: We included 1,584 participants (mean age, 76.1 ± 7.5; range 52-102 years; 56% female), of whom 52% had chronic pain, 36% had chronic multisite pain, 15.6% had chronic WSP, and 10.4% B-HICP (Figure 1). Prevalence of either chronic multisite or WSP did not increase with age (p>0.05; Figure 1). However, pain impact—as measured by pain interference and percent whose pain classified as B-HICP—did increase with age for women (both p< 0.05; Figures 1 & 2).
Conclusion: Our findings suggest that although pain does not become more widespread with advancing age in either men or women, pain burden does increase with age in women. Thus, similar numbers of pain sites contribute to a greater level of pain burden in oldest-old women than it does in younger-old counterparts. Pain impact measures that incorporate pain frequency, intensity, and pain interference, may better reflect burden than number of pain sites, especially among older women.
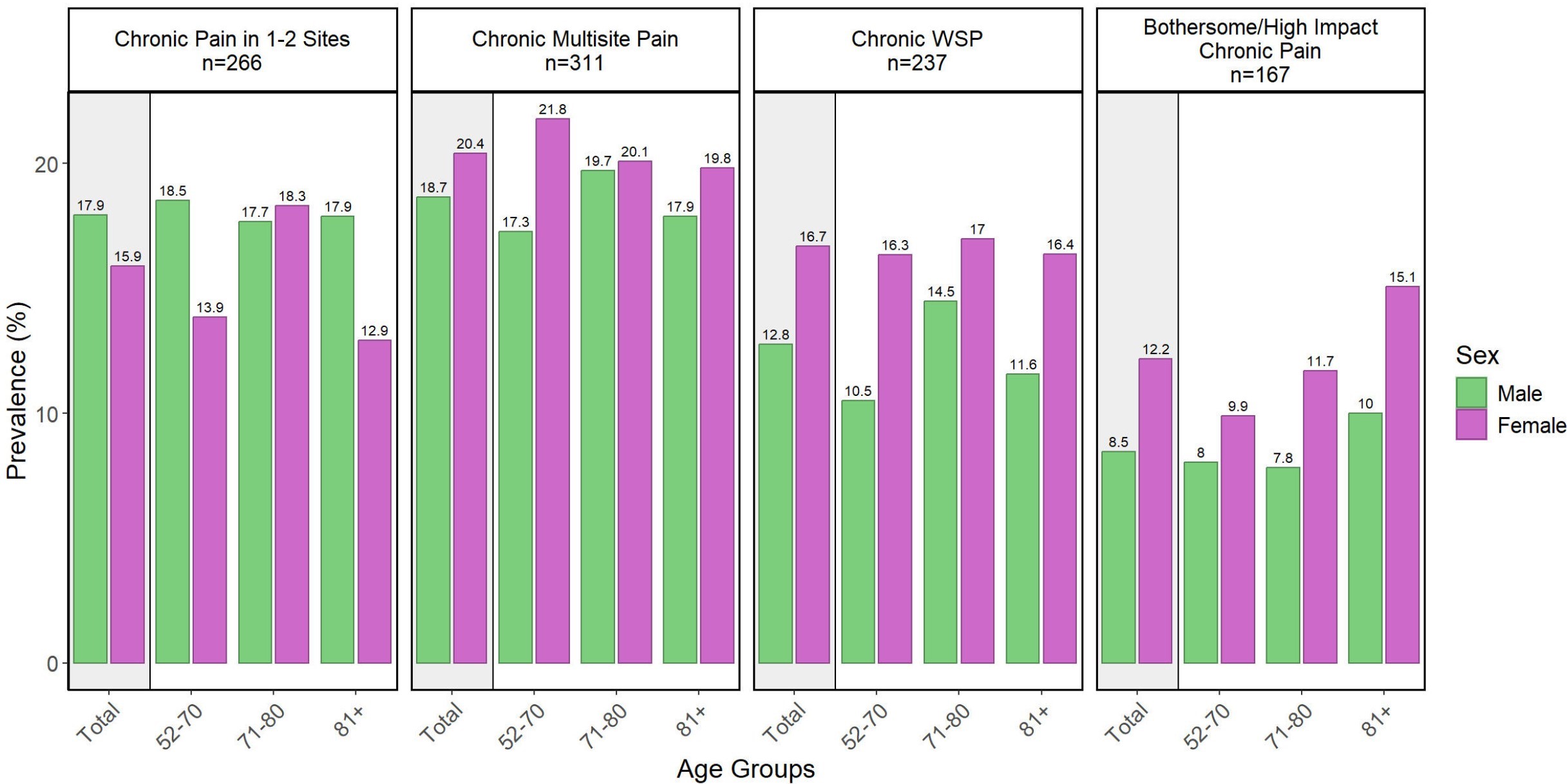 Figure 1: Pain prevalence by classification, stratified by age and sex.
Figure 1: Pain prevalence by classification, stratified by age and sex.
.jpg) Figure 2: Pain interference score by pain classification, stratified by age and sex.
Figure 2: Pain interference score by pain classification, stratified by age and sex.
To cite this abstract in AMA style:
Fennell G, Tilley S, Dhamne S, Demalia A, Clancy M, Gheller M, Edwards R, Benjamin E, Neogi T. Extent versus impact: Sex-specific burden of chronic pain in older adults [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/extent-versus-impact-sex-specific-burden-of-chronic-pain-in-older-adults/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/extent-versus-impact-sex-specific-burden-of-chronic-pain-in-older-adults/
