Session Information
Date: Monday, October 27, 2025
Title: (1147–1190) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: VEXAS syndrome is an adult-onset autoinflammatory disorder caused by somatic mutations in UBA1 gene, characterized by systemic inflammation and haematologic abnormalities. Evidence regarding its evolution and approach in real-world settings remains limited.To aim of this study is to evaluate the clinical progression, inflammatory markers, and treatment response in patients with VEXAS syndrome over a 3, 6, and 12 month-period following diagnosis.
Methods: Observational, ambispective study involving patients with a genetic diagnosis of VEXAS syndrome across rheumatology units in Spain. Follow-up data at 3, 6, and 12 months were collected, including demographic, clinical, laboratory, and treatment related variables. Response rate was defined as complete (RC) (no VEXAS symptoms, CRP ≤10mg/L, prednisone ≤10mg qd), partial (PR)(clinical remission, CRP and prednisone reduction ≥50%) or none (N) (ongoing symptoms, persistent inflammatory markers, no steroid reduction).
Results: Fifty patients (n=50) were identified. Follow-up data were available for 25 patients at 3 months, 24 at 6 months, and 19 at 12 months. On the one hand, VEXAS syndrome hallmark symptoms (skin lesions, constitutional syndrome, arthritis, thromboembolic disease, pulmonary and renal involvement) decreased over time (”Table 1”). On the other hand, inflammatory markers (CRP, ESR) and haemoglobin levels showed scarce to moderate non-significant improvement. Macrocytosis (MCV > 100 fL) remained persistently elevated (“Figure 1”).At the moment of diagnosis, most frequently prescribed treatments were glucocorticoids (GCs) (92%), azacitidine (28%), MTX and JAK inhibitors (24%), IL-6 inhibitors (16%), and anakinra (18%).At 3 months, GCs remained the predominant choice of treatment (92%), though both CR and PR were estimated at 38.1%. JAK inhibitors (12%) showed 50% complete response, while IL-6 inhibitors (8%) showed 50% CP and PR response. MTX (16%) showed 75% PR. Anakinra (8%) induced only PR.At 6 months, glucocorticoids were used in 100% of patients (31.8% CR, 50% PR). IL-6 and JAK inhibitors (both 16.16%) showed 25% CR and 75% PR. MTX (12.5%) maintained a 66.7% PR. Azacitidine (12.5%) showed limited efficacy.At 12 months, glucocorticoids (100%) continued with 31.8% CR and 50% PR. JAK and IL-6 inhibitors (21.05% each) maintained similar response profiles. MTX (15.58%) still showed 66.7% partial response. Anakinra and azathioprine were discontinued (“Table 2”). Two 2 patients underwent allo-HCT, with CR in one case (50%). It has not been possible to lower GCs below 10 mg/day in 1 of the cases after 12 months (partial response 50%).
Conclusion: This multicenter, ambispective study provides real-world data on the disease course and treatment of VEXAS syndrome. GCs remain essential, but seem to lose efficacy over time. IL-6 and JAK inhibitors, especially Ruxolitinib, appear to offer sustained benefit. Despite intensive immunosuppression, inflammatory and haematologic activity persists in many patients. HSCT is a feasible option in selected cases.
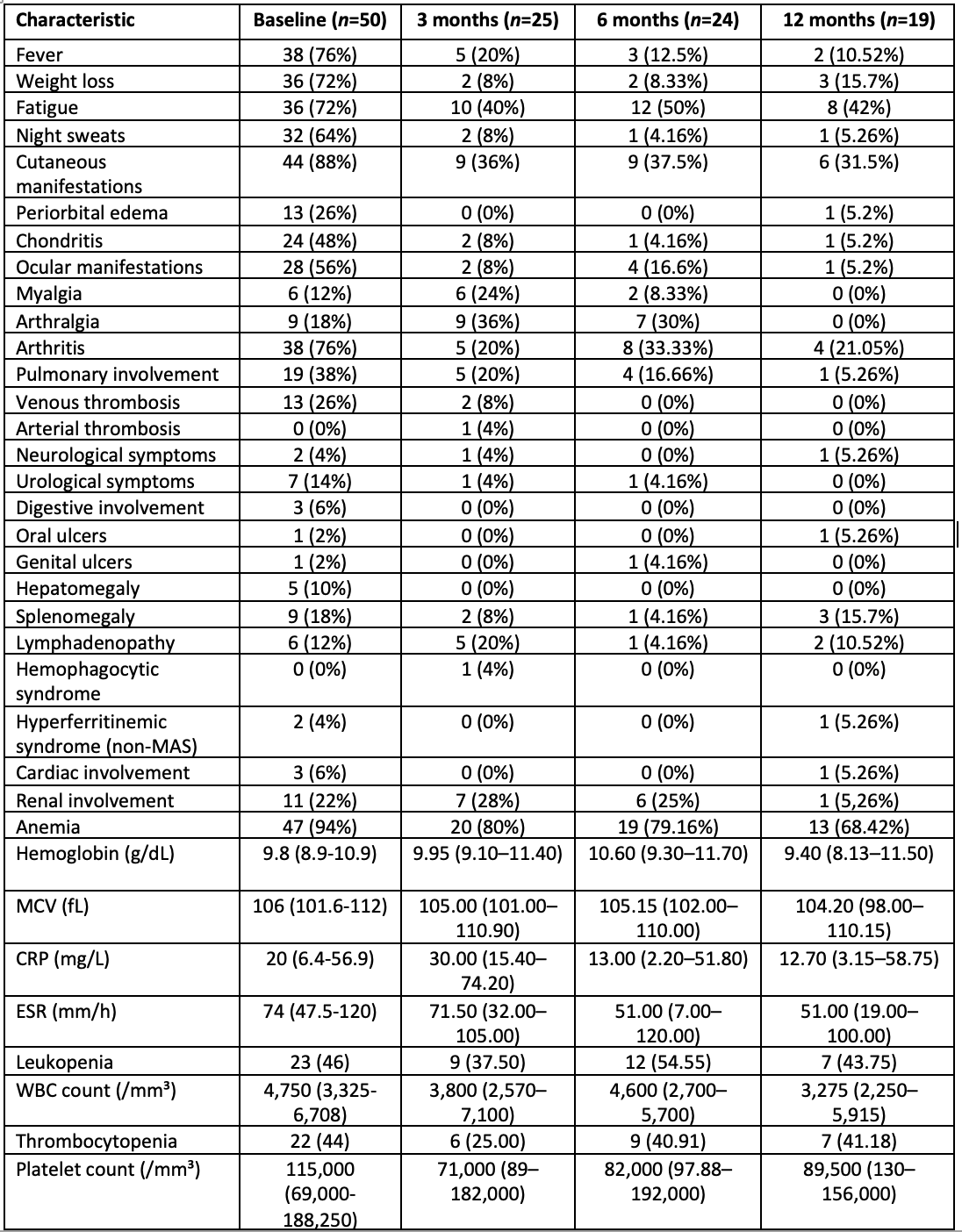 Table 1. Baseline and follow-up clinical features at 3, 6, and 12 Months
Table 1. Baseline and follow-up clinical features at 3, 6, and 12 Months
.jpg) Figure 1. Longitudinal Trends in Inflammatory and Hematologic Biomarkers in Patients with VEXAS Syndrome
Figure 1. Longitudinal Trends in Inflammatory and Hematologic Biomarkers in Patients with VEXAS Syndrome
.jpg) Table 2. Longitudinal Overview of Therapies Used and Frequency at 0, 3, 6, and 12 Months
Table 2. Longitudinal Overview of Therapies Used and Frequency at 0, 3, 6, and 12 Months
To cite this abstract in AMA style:
López M, Garcia Escudero P, Magallares B, Salles Lizarzaburu M, Fiallo Suárez D, Rúa-Figueroa I, Morante Bolado I, Aurrecoechea E, Enriquez E, Merino C, Castañeda S, Monjo Henry I, Egües Dubuc C, Oliver García E, Garcia A, Font-Urgelles J, Corrales C, Villalobos L, Boteanu A, Vázquez Gómez I, Dios D, Garcia Belando C, Frade Sosa B, Reina D, Ibañez M, Carrion I, Rodriguez M, Sieiro c, Toyos F, Mariano A, Moriano C, Melero-González R, Vela Casasempere P, Miranda J, Boselli G, Hernandez J, Trallero E, Riera Alonso E, Calvo J. VEXAS Syndrome Under the Lens: A prospective analysis of temporal disease patterns, biomarker Dynamics, and therapeutic efficacy [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/vexas-syndrome-under-the-lens-a-prospective-analysis-of-temporal-disease-patterns-biomarker-dynamics-and-therapeutic-efficacy/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/vexas-syndrome-under-the-lens-a-prospective-analysis-of-temporal-disease-patterns-biomarker-dynamics-and-therapeutic-efficacy/
