Session Information
Date: Monday, October 27, 2025
Title: (1147–1190) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: VEXAS syndrome is a recently described, adult-onset autoinflammatory disease caused by somatic mutations in the UBA1 gene, typically affecting hematopoietic stem cells. Renal involvement was not prominently featured in early reports. The pathophysiology of VEXAS-associated kidney disease is not yet fully understood, but it is hypothesized that the UBA1-mutant myeloid clone directly infiltrates and damages renal tissue, as cytoplasmic vacuoles and UBA1-mutant cells have been identified in affected organs. Given that renal complications can lead to substantial morbidity, recognizing and characterizing kidney involvement in VEXAS is crucial.This review provides a comprehensive synthesis of the literature since VEXAS was first described, focusing on renal manifestations, biopsy findings, the frequency of kidney involvement, treatments used, and outcomes.
Methods: We searched PubMed/MEDLINE and Google Scholar for original articles with patient level data from 2020 on renal involvement in VEXAS syndrome. Key data was extracted from each report manually.The PRISMA diagram is shown below (Figure 1)
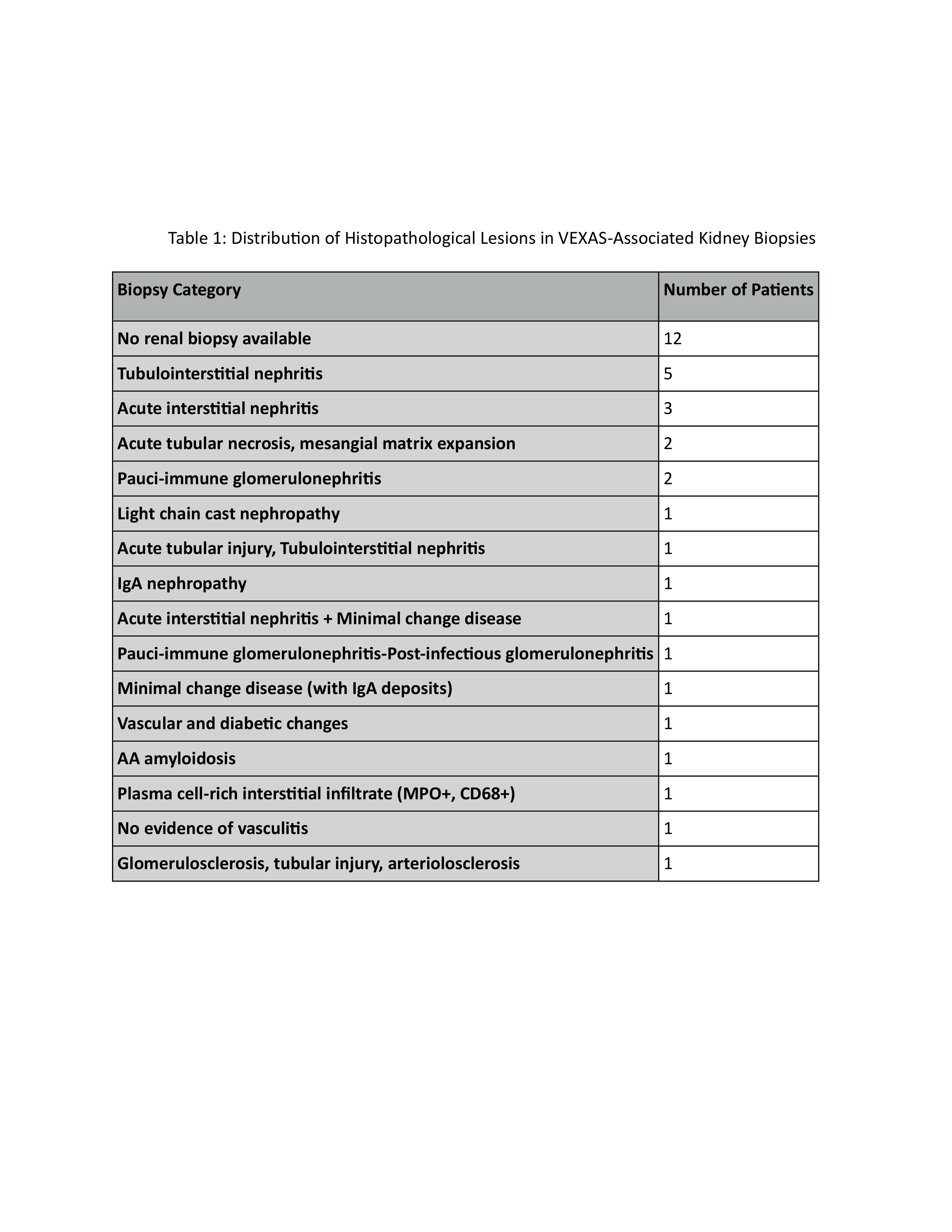
Results: Kalantari et al. found AKI incidence of 6.2% at 1 year and 39% by year 10. A Dutch series showed 2 of 12 men had renal involvement; a Swiss series had 1 of 17 with AKI. In a French study, only 11 of 303 patients (3.6%) underwent biopsy. True prevalence may be higher due to avoided biopsies and empirical treatment.Patients (all male, aged 47–86) presented with CKD or abrupt AKI. Proteinuria was common; 5 of 11 French cases had nephrotic-range proteinuria. Hematuria and pyuria occurred in ~50%. Table 1 summarises biopsy findings.The association with VEXAS flares was unclear—only 3 of 11 had flare-associated AKI. However, AKI often improved with immunosuppression. CRP elevation correlated with AKI onset in the Mayo cohort. Glucocorticoids remain first-line. In the Mayo cohort, all responded with improved kidney function and inflammation. Relapses with tapering necessitated steroid-sparing agents: cyclophosphamide, methotrexate, azathioprine, MMF. Targeted agents (tocilizumab, anakinra, JAK inhibitors) were used in refractory cases. Azacitidine may reduce inflammation by suppressing mutant clones. HSCT may induce remission; of two Mayo cases, one recovered, one had stable CKD post HSCT.AKI often improved with treatment; dialysis was rare.The role of renal disease in mortality remains unclear.
Conclusion: Kidney involvement in VEXAS can take diverse forms—most commonly interstitial nephritis and vasculitic glomerulonephritis, often parallel the activity of the systemic disease. Biopsy findings of plasma cell and neutrophil infiltration in the kidneys, along with UBA1 mutation positivity, suggest direct tissue damage by infiltrating mutant myeloid clones.The mainstay of treatment for VEXAS flares, including renal involvement, is glucocorticoids. Adjunctive therapies are frequently added. Renal prognosis following HSCT has been favorable in the two patients with AKI reported. Mortality and dialysis dependence are rarely observed.Ongoing research is needed to better understand why certain VEXAS patients develop renal involvement and to establish optimal treatment algorithms.
.jpg) Table 1: Distribution of Histopathological Lesions in VEXAS-Associated Kidney Biopsies
Table 1: Distribution of Histopathological Lesions in VEXAS-Associated Kidney Biopsies
To cite this abstract in AMA style:
Perumangote Vasudevan A, Mulavini V, Hashim R, Rondla M, C Unnikrishnan D. Renal Manifestations in VEXAS Syndrome: A Systematic Review of Clinical Features, Pathology, and Outcomes [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/renal-manifestations-in-vexas-syndrome-a-systematic-review-of-clinical-features-pathology-and-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-manifestations-in-vexas-syndrome-a-systematic-review-of-clinical-features-pathology-and-outcomes/