Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Recognizing health care disparities in Rheumatoid Arthritis is crucial to improving outcomes. This study analyzes factors contributing to RA care inequities.
Methods: We examined RA disease activity, treatment, and vaccine rates over 12 yearly periods, 2012-2023. Eligibility criteria included RA patients ≥18 years. Low Clinical Disease Activity Index (CDAI≤10), steroid use ≥3 months, DMARD use ≥6 months, and vaccine (pneumococcal, shingles, flu) rates were compared based on insurance types and gender. Generalized estimating equations regression models were used to analyze binomial/multinomial outcomes.
Results: Population included 24,469 patients, median age 63, white 96%, women 74%, RF+ 74%, anti-cyclic citrullinated peptide (CCP+) 28%, Medicare 49%, Medicaid 5%, and Commercial insurance 22%. Insurance type didn’t affect DMARD use: Commercial versus (vs) Medicare and Medicaid (Odds Ratio (OR) 0.98, 0.97, p=0.7936, p=0.8242), Medicaid vs Medicare (OR 1.01, p=0.9426) (Figure 1). More women used DMARDs than men (OR 1.22, p=0.0074) (Figure 2). Steroid use was higher with Medicaid than Medicare and Commercial patients (OR 1.25, 1.41, p=0.0128, p=0.0003) respectively (Figure 1), and higher in men than women until period 9 (p=0.0002) (Figure 2). Disease control was better with Medicare and Commercial than Medicaid patients (OR 2.39, 2.22, p=0.001 respectively) but worse over time for all insurances (70.34% to 59.14%, p< 0.0001) (Figure 1). Men started with lower rates of CDAI ≤10 than women in period 1 (62% vs 71%) but achieved greater low disease activity than women in periods 2-12 (68% vs 59% p=0.046) (Figure 2). Disease activity worsened post COVID-19 pandemic for both insurance and gender in period 9 (2020) to 12 (2023) (Figures 1,2). Vaccine rates were higher with Medicare than Commercial or Medicaid (Singles OR 2.51, 3.28 p< 0.0001), (Pneumococcal OR 2.31, 2.33 p=0.0001), (Flu OR 1.41, 2.59 p=0.0001) (Figure 3). Pneumococcal and flu vaccine rates declined over time for all insurances (69% to 58%, 72% to 52%, p=0.0185, p=0.0001 respectively) (Figure 3). Gender didn’t influence vaccine rates, but they all declined with time (p< 0.05) (Figure 3). The decline in vaccination trend was particularly worsened post COVID-19 (period 9-12) independent of insurance or gender (Figure 3). Comparing to national data, our vaccine rates were similar for flu (53-72% vs 61%) (Coca, Arth. Rheumatol.2018;70(9)) but superior for shingles (39-46% vs 19%) (Calabrese, Arth. Care Res.2020;72(3)), and pneumococcal (58-69% vs 43%) (Alvarez, Vaccine.2024;42(3)).
Conclusion: Insurance type, gender, and COVID-19 played a substantial role in RA care delivery. Higher vaccine rates were achieved with Medicare, however, an overall declining trend, worse post COVID-19, left a considerable gap in our RA patients. Men (period 1-9) and Medicaid patients used more steroids. Men used less DMARDs, while percent at low disease activity worsened for all patients over time. This may be due to a higher capture of elevated CDAI measures (requires an in person visit) during COVID-19 (when the sickest patients were seen in person). Recognizing the drivers of RA inequities provides us with the opportunity to use a targeted approach to improving care.
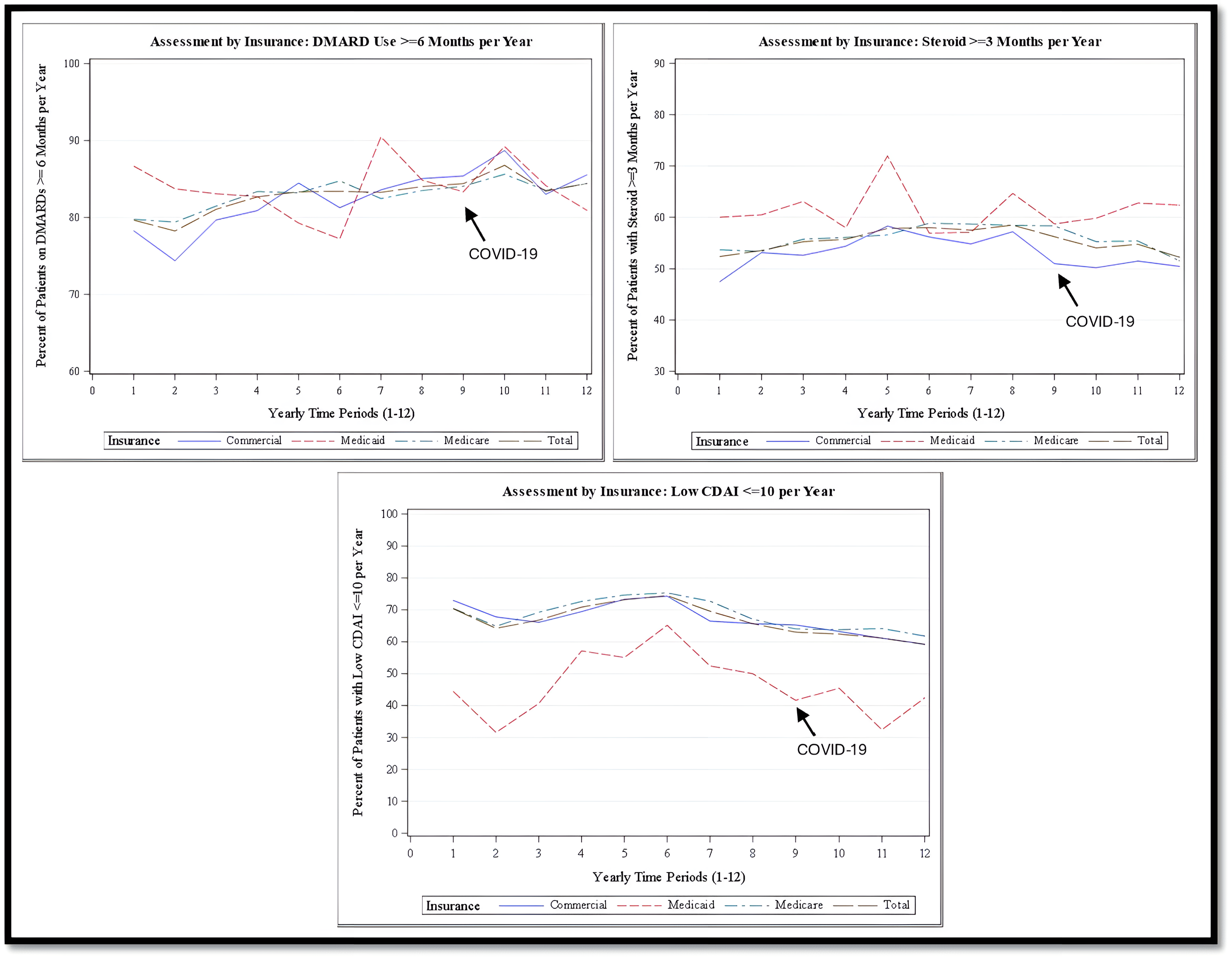 Figure 1. The Treatment Rates (DMARD ≥6 months, Steroids ≥3 months) and Disease Activity (Low CDAI ≤10) Assessment by Insurance Type
Figure 1. The Treatment Rates (DMARD ≥6 months, Steroids ≥3 months) and Disease Activity (Low CDAI ≤10) Assessment by Insurance Type
.jpg) Figure 2. The Treatment Rates (DMARD ≥6 months, Prednisone ≥3 months) and Low Disease Activity (CDAI ≤10) Assessment by Gender
Figure 2. The Treatment Rates (DMARD ≥6 months, Prednisone ≥3 months) and Low Disease Activity (CDAI ≤10) Assessment by Gender
.jpg) Figure 3. The Vaccine Rates (Shingles, Flu, and Pneumococcal) Assessment by Insurance types and Gender
Figure 3. The Vaccine Rates (Shingles, Flu, and Pneumococcal) Assessment by Insurance types and Gender
To cite this abstract in AMA style:
Riaz R, Zhang L, Berger A, Srinivasan H, Schroeder L, Cote J. Insurance, Gender, and COVID-19’s Effects on Health Inequity in Rheumatoid Arthritis: A 12-Year Long Population Assessment [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/insurance-gender-and-covid-19s-effects-on-health-inequity-in-rheumatoid-arthritis-a-12-year-long-population-assessment/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/insurance-gender-and-covid-19s-effects-on-health-inequity-in-rheumatoid-arthritis-a-12-year-long-population-assessment/
