Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Although studies have been published on the baseline characteristics of patients with autoimmune rheumatic diseases (AIRDs) with COVID-19 infection, little data exists on how social determinants of health (SDoH) influence outcomes. We investigated whether specific domains of SDoH are associated with COVID-19-related hospitalizations in adults with and without AIRDs.
Methods: We conducted a retrospective cohort study using electronic health record (EHR) data from the National Clinical Cohort Collaborative (N3C) COVID Enclave. We included adults ≥18 years who tested positive for SARS-CoV-2 (PCR or antigen test or diagnostic code) between April 2020 and March 2024. We identified patients with AIRD by the presence of ≥2 ICD-10 codes for an AIRD diagnosis, recorded ≥ 30 days apart before an incident COVID-19 infection. The AIRD diagnoses we included were polymyalgia rheumatica, polymyositis, dermatomyositis, rheumatoid arthritis, systemic sclerosis, ankylosing spondylitis, psoriatic arthritis, enteropathic arthritis, reactive arthritis, Behcet’s disease, ANCA-vasculitis, giant cell arteritis, polyarteritis nodosa, SLE, and Sjogren’s syndrome. Only individuals with available SDoH data in N3C were included in this study and SDoH were assessed at the time of incident COVID-19 infection. SDoH were assessed across three Healthy People 2030 domains: healthcare access, economic stability, and social cohesion. The primary outcome was COVID-19-related hospitalization defined as occurring within a window from 3 days before to 14 days after diagnosis. To examine the association between specific SDoH domains and COVID-19-related hospitalization among adults with and without AIRDs, we conducted hierarchically nested logistic regression models and adjusted for covariates including age, sex, comorbidities, and vaccination status, then stratified analyses by AIRD status.
Results: There were 362,359 people with incident COVID-19 infection and available SDoH domains in N3C at the end of data collection, of whom 16,261 (4.5%) had at least one AIRD diagnosis. In unadjusted analyses, COVID-19-related hospitalization was significantly higher among AIRD patients (19%) compared to non-AIRD patients (13%, p < 0.001; Table 1). Across both AIRD and non-AIRD groups, having SDoH issues was associated with higher odds of COVID-19-related hospitalization (Table 2). In adjusted models including all SDoH domains, associations were consistently stronger among the AIRD group. Having access to healthcare issues was associated with higher hospitalization risk in both groups, with a larger effect in AIRD patients (aOR 1.73, 95% CI 1.41-2.11) than in non-AIRD patients (aOR 1.55, 95% CI 1.45-1.66). Similarly, social cohesion issues (aOR 1.44 vs 1.19) and economic instability (aOR 1.20 vs 1.16) had a more pronounced association with hospitalization in the AIRD group (Table 2).
Conclusion: Having SDoH issues was independently associated with higher odds of COVID-19-related hospitalization among adults, regardless of AIRD status. These associations were stronger in those with AIRDs, highlighting how underlying social disadvantage may exacerbate vulnerability to severe outcomes in this population.
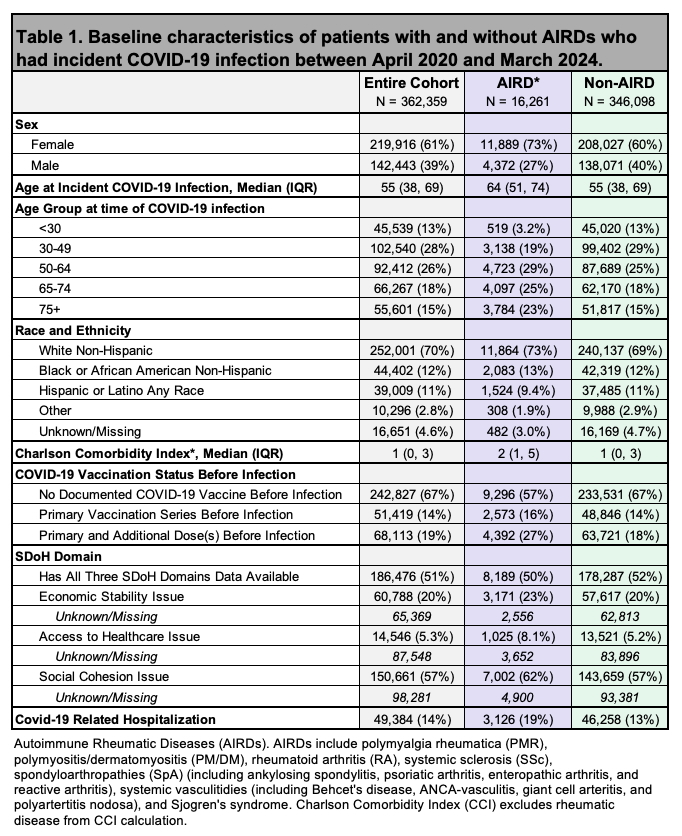 Table 1. Baseline characteristics of patients with and without AIRDs who had incident COVID-19 infection between April 2020 and March 2024.
Table 1. Baseline characteristics of patients with and without AIRDs who had incident COVID-19 infection between April 2020 and March 2024.
.jpg) Table 2. Odds of COVID-19-related hospitalization among Social Determinates of Health (SDoH) domains, stratified by presence of AIRD. Adjusted covariates included age, sex, comorbidities, and COVID-19 vaccination status prior to incident infection.
Table 2. Odds of COVID-19-related hospitalization among Social Determinates of Health (SDoH) domains, stratified by presence of AIRD. Adjusted covariates included age, sex, comorbidities, and COVID-19 vaccination status prior to incident infection.
To cite this abstract in AMA style:
Robinson L, anzalone j, Singh J, Michaud K, Jackson L, Danila M, Li D, Patel R, Singh N. Association Between Social Determinants of Health Domains and COVID-19-Related Hospitalization in Individuals with Autoimmune Rheumatic Diseases: A Retrospective Analysis of National U.S. Data [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-between-social-determinants-of-health-domains-and-covid-19-related-hospitalization-in-individuals-with-autoimmune-rheumatic-diseases-a-retrospective-analysis-of-national-u-s-data/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-social-determinants-of-health-domains-and-covid-19-related-hospitalization-in-individuals-with-autoimmune-rheumatic-diseases-a-retrospective-analysis-of-national-u-s-data/
