Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease with multi-organ involvement that is characterized by relapses and remissions. Ethnicity, socioeconomic status, gender, age, education level, and healthcare access are associated with poorer disease outcomes among patients with SLE. The social vulnerability index (SVI), developed by the Centers for Disease Control and Prevention (CDC), is a measure of demographic and socioeconomic factors that adversely affect health outcomes. We aim to determine the association between SVI and mortality in our lupus cohort.
Methods: This was a single-center retrospective study of all SLE patients hospitalized at the University of Rochester Strong Memorial Hospital between July 2016 and June 2023. We analyzed the age, race and ethnicity, mortality, and SVI among all those hospitalized. SVI is measured on a percentile ranking from 0 to 1, with higher percentiles indicating more social vulnerability. Additionally, SVI is divided into 4 subcategories (socioeconomic status, household characteristics, racial & ethnic minority status, and housing type & transportation) which are also assessed on a percentile scale from 0 to 1. The SVI and the scores of the 4 subcategories were determined based on publicly available CDC data and the patient’s current addresses. The ANOVA and chi-squared tests were used to assess differences in demographic risk factors and mortality. The Cox regression was used to assess the hazard ratios for SVI and its subcategories.
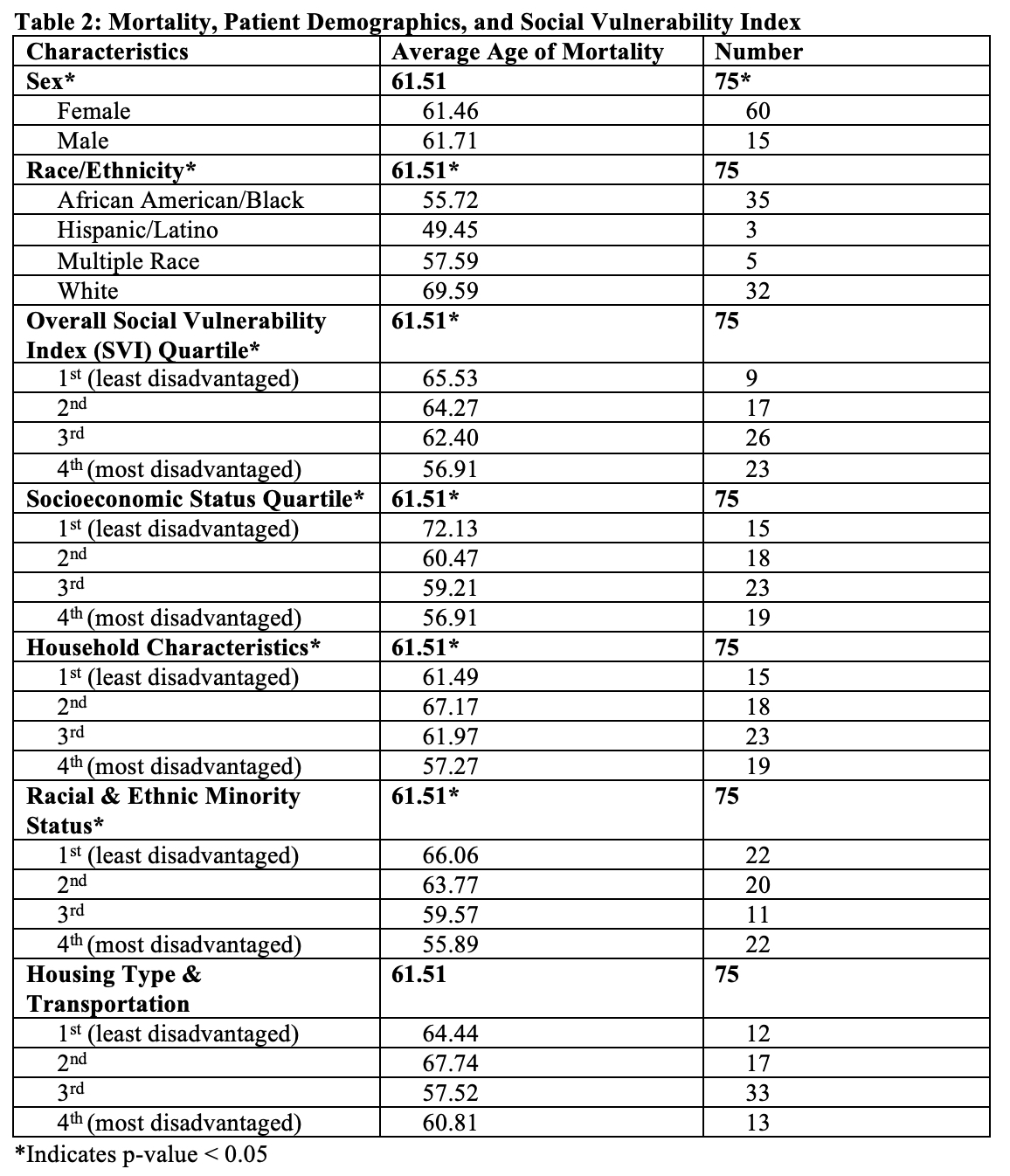
Results: A total of 405 patients met criteria for a diagnosis of SLE. There were 75 deaths during the specified time period (Table 1). The mean age of death for the entire cohort was 61.51 years. The mean age of death for those patients identifying as White was 69.59 years, 55.72 years for Black patients, and 49 years for Hispanic patients (p-value = 0.0019) (Table 2). Although the age of mortality was not significantly different between females and males (61.46 vs 61.71 years, p-value = 0.9583), there was a significant difference in mortality rates (16.6% in females vs 34.9% in males, p-value = 0.0035). The average age of death of patients in the first quartile of SVI was 65.53 years of age compared to 56.81 years of age for patients in the last quartile of SVI. Patients of higher social vulnerability had a significantly higher risk of death with a hazard ratio of 3.38 (p-value = 0.004) (Table 2, Figure 1). Higher percentile scores were associated with significantly higher risk of death for all subcategories of SVI, except for housing type & transportation (Table 2, Figure 1).
Conclusion: There is a significant difference in age of mortality among hospitalized SLE patients based on race. Additionally, patients with a higher social vulnerability score are at a higher risk of death. Among the four subcategories of social vulnerability, socioeconomic status, household characteristics, racial & ethnic minority status contributed to significantly increased risk of death while housing type & transportation did not. Providing additional care and developing specific interventions to overcome barriers to care may help reduce mortality among lupus patients with high SVI scores.
To cite this abstract in AMA style:
Kim C, Mitchell K, Feng C, Anandarajah A. Demographic Risk Factors, Social Vulnerability Index, and Mortality in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/demographic-risk-factors-social-vulnerability-index-and-mortality-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/demographic-risk-factors-social-vulnerability-index-and-mortality-in-patients-with-systemic-lupus-erythematosus/

.jpg)
.jpg)