Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Guidelines recommend limiting glucocorticoid (GC) use in RA, but 30% of patients continue long-term GCs. Little is known about the influence of provider attitudes and characteristics on prescribing patterns. We conducted a provider survey nested within a RA registry to identify provider factors associated with GC use.
Methods: A survey was sent to providers contributing patients to the prospective, observational, CorEvitas Rheumatoid Arthritis registry, capturing demographics, provider concerns about the safety of different medications, and a range of healthcare-related and non-healthcare related beliefs. We then identified patients with RA initiating a new biologic or Janus kinase inhibitor (JAKi) who remained on the same therapy at a 6 month follow-up visit, using the first qualifying observation per patient. Patient factors associated with GC use 6 months after treatment initiation were assessed using a mixed effects logistic regression model clustered by provider. Similar models limited to patients of the survey responders assessed whether different provider characteristics and beliefs were associated with GC prescribing 6 months after treatment initiation, adjusting for patient factors. All models were weighted for number of patients per provider.
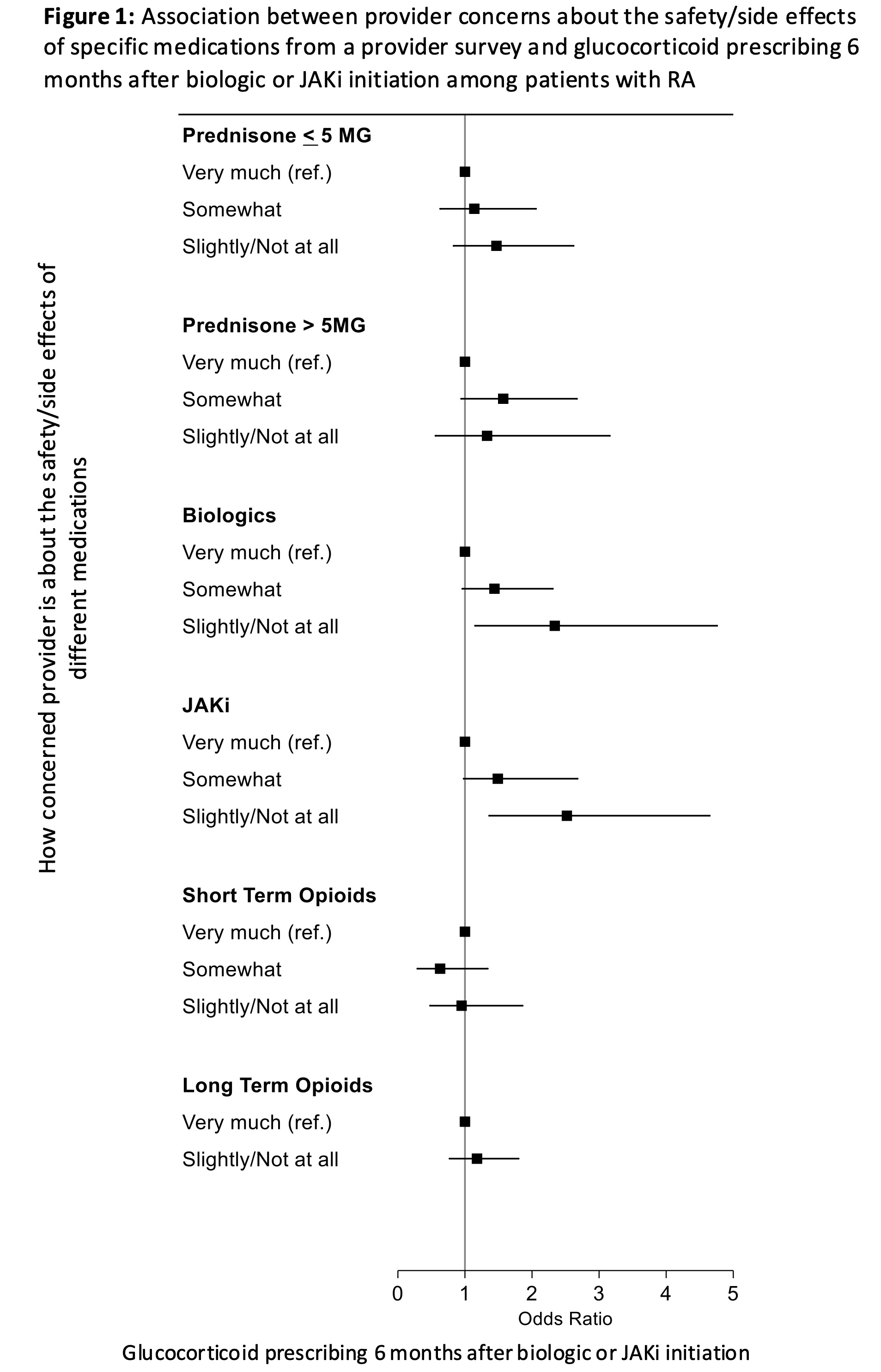
Results: Among 256 active providers contributing patients to the registry, 92 (36%) responded to the survey and 81 had patients meeting all inclusion criteria. These 81 responders had 3966 qualifying patients, while 164 non-responders had 3219 qualifying patients. Among all 7185 patients, higher baseline disease activity, less improvement at 6 months, age ≤45 or >75, more long-standing RA, more previous biologics/JAKi, and earlier calendar year were associated with greater GC use at 6 months (Table 1). Patients of survey responders were less likely to use GCs (OR 0.68, CI 0.049-0.94), and 13% of the variability in GC use was due to provider. In analyses limited to survey responders: provider demographics, burnout, and beliefs regarding shared decision making, complementary/alternative medications, race as a biologic factor in medicine, political leanings, and religiosity were not associated with GC prescribing (Table 2). As shown in Figure 1, concerns about long-term prednisone ≤5mg or >5mg or opioids were not associated with GC prescribing, but providers with less concern about biologics or JAKi were more likely to prescribe GCs at 6 months [adjusted OR 2.34 (1.15-4.76) for biologics, OR 2.52 (1.36-4.65) for JAKi for slightly/not at all vs. very much concerned].
Conclusion: While patient factors have a strong influence on GC use in RA, variability in practice patterns among providers also impacts GC use. Many provider characteristics and beliefs, and surprisingly even concerns about GCs, are not associated with GC prescribing. In contrast, providers with less concern about biologics and JAKi are more likely to prescribe GCs. These results suggest that broader attitudes towards prioritizing treatment benefits vs risks may drive GC prescribing, with important implications for provider education.
To cite this abstract in AMA style:
George M, Reed G, Kane K, Pappas D, Kremer J. Provider Characteristics and Beliefs and Patient Factors Associated with Long-term Glucocorticoid Use in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/provider-characteristics-and-beliefs-and-patient-factors-associated-with-long-term-glucocorticoid-use-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/provider-characteristics-and-beliefs-and-patient-factors-associated-with-long-term-glucocorticoid-use-in-patients-with-rheumatoid-arthritis/

.jpg)
.jpg)