Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatology consults are often obtained in hospitalized patients with known or suspected rheumatologic disease. Identifying factors linked to poor short-term outcomes may improve risk stratification during hospitalization and post-discharge planning. This study aimed to characterize demographic, clinical, and social factors associated with 30-day readmission or in-hospital death in patients receiving a rheumatology consult.
Methods: We conducted a retrospective cohort study of patients hospitalized at Barnes Jewish Hospital (Saint Louis, MO) from 4/1/2024-9/30/2024 who received an inpatient rheumatology evaluation for confirmed or suspected rheumatologic conditions. Variables of age, sex, Area Deprivation Index (ADI), disabilty status were collected. Clinical data such as rheumatologic diagnosis, comorbidities (infection, CAD, hypertension) and length of stay (LOS) were collected. The primary outcomes were in-hospital mortality and 30-day all-cause readmission. Associations were assessed using chi-square tests, and independent predictors were evaluated via binary logistic regression. Statistical significance was set at p < 0.01 for chi-square and < 0.02 (Bonferroni-Hochberg adjusted) for regression.
Results: Among 268 rheumatology consult patients, 36 (13.4%) were readmitted within 30 days and 19 (7.1%) died during admission. Analyses showed higher readmission rates among those with disability (χ² = 11.389, p < .001 [all listed are unadjusted]) and a trend with CAD (χ² = 2.648, p = .104). Infections were more common among patients who died (χ² = 7.449, p < .006), with a trend toward male predominance (χ² = 2.714, p = .099). Logistic regression confirmed disability as the only significant predictor of readmission (OR = 4.16, p = .001), with male sex trending toward significance (OR = 1.97, p = .105). Death during admission was significantly associated with longer length of stay (OR = 1.11, p = .020), while age was borderline, just falling outside the corrected cut-off of p < 0.02 (OR = 1.06, p = .022). Infection (OR = 1.20, p = .081) and lower ADI (OR = 0.31, p = .080) also showed non-significant trends towards death during admission.
Conclusion: In this cohort, disability status was associated with more than a four-fold risk of 30-day readmission. Other factors such as male sex, known CAD also trended towards higher readmission risk. When looking at deaths during the index admission, LOS and age, alongside presence of infection, was more relevant. Notably, a lower ADI was linked (not significantly) with increased odds of death. This preliminary study highlights the importance of targeted post-discharge planning for patients with disabilities to reduce possible early rehospitalization alongside further research regarding comprehensive mortality risk stratification.
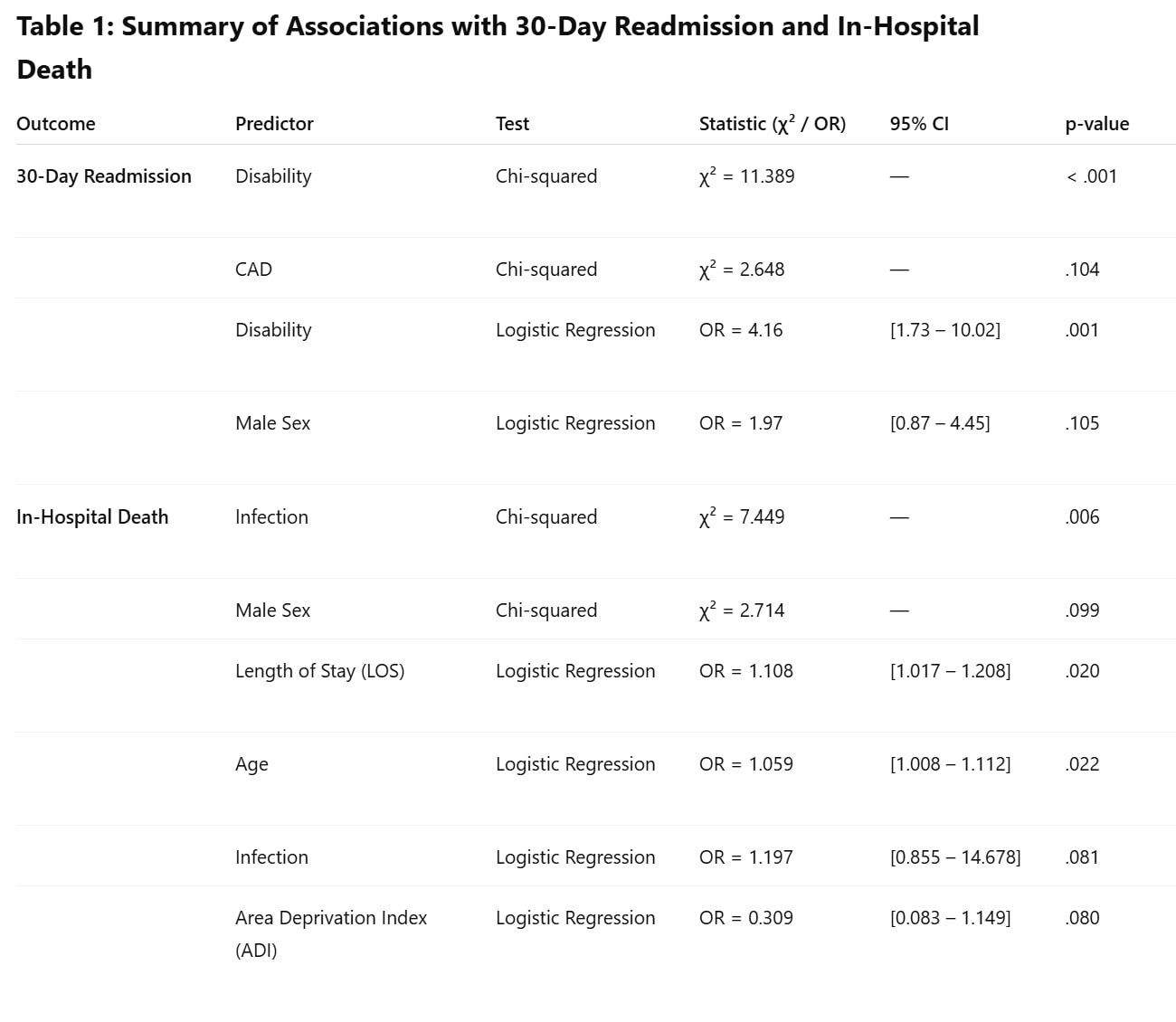 Summary of Chi-Squared and Logistical Regression Analysis for selected variables
Summary of Chi-Squared and Logistical Regression Analysis for selected variables
To cite this abstract in AMA style:
Ali W, Sen D. Demographic and Clinical Correlates of 30 day Re-admission or Death During Admission in Patients With Rheumatologic Conditions : A Retrospective Cohort Analysis in a Single Academic Center [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/demographic-and-clinical-correlates-of-30-day-re-admission-or-death-during-admission-in-patients-with-rheumatologic-conditions-a-retrospective-cohort-analysis-in-a-single-academic-center/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/demographic-and-clinical-correlates-of-30-day-re-admission-or-death-during-admission-in-patients-with-rheumatologic-conditions-a-retrospective-cohort-analysis-in-a-single-academic-center/
