Session Information
Date: Sunday, October 26, 2025
Title: (0671–0710) Systemic Sclerosis & Related Disorders – Clinical Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with systemic sclerosis (SSc) face increased cancer risk compared to the general population, yet current evidence on specific cancer patterns and their relationship to autoantibody status remains poorly characterized. We investigated cancer risk patterns in systemic sclerosis (SSc) patients and investigate associations between specific autoantibodies and cancer development.
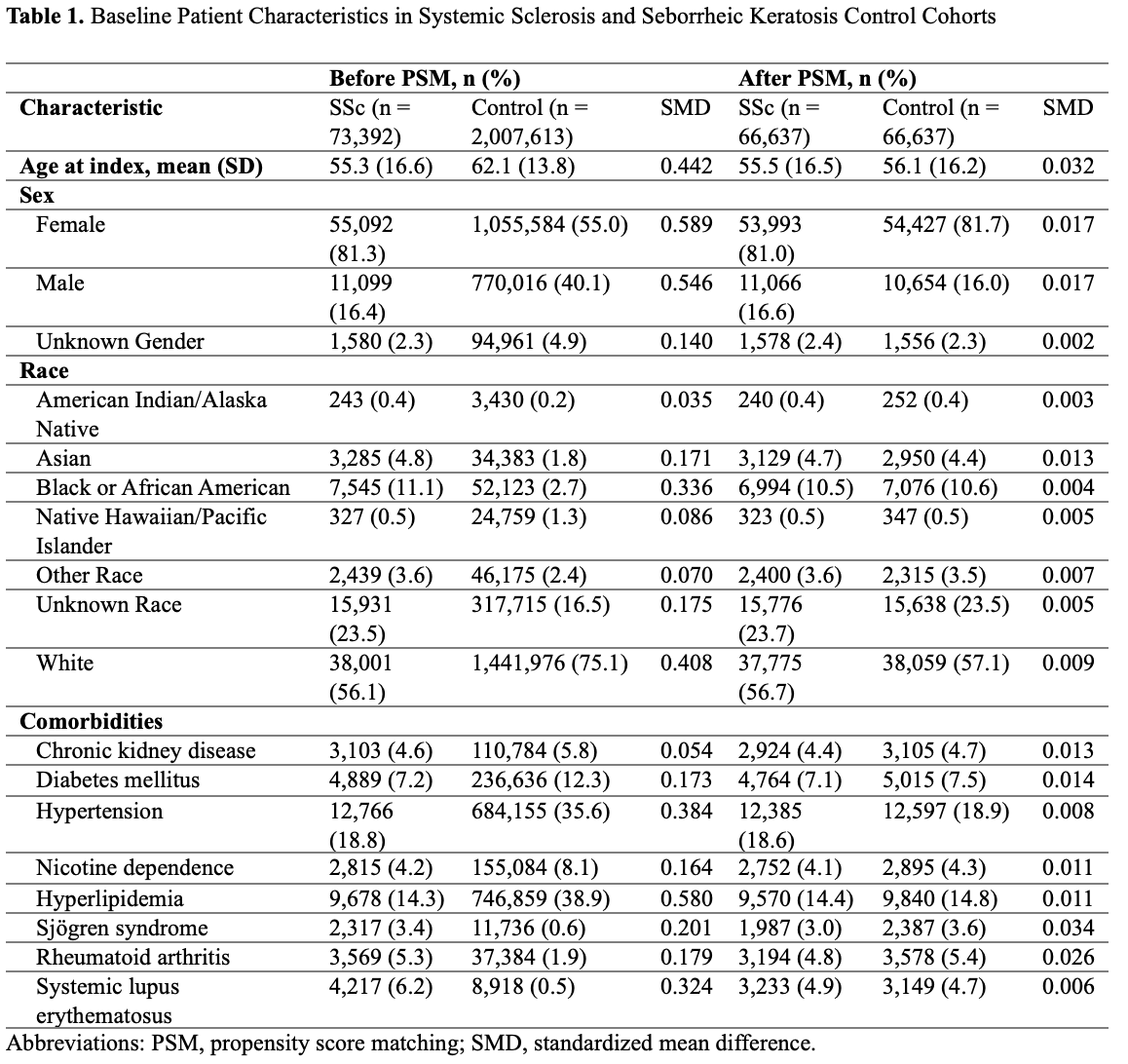
Methods: This multi-center cohort study analyzed 5-year cancer incidences in adults with SSc versus matched controls with seborrheic keratosis using electronic medical record data from 128 healthcare organizations (from 2016-2024) in the TriNetX platform, a Health Insurance Portability and Accountability Act and General Data Protection Regulation-compliant federated research network. Patients were stratified by autoantibody status (anti-Scl-70, RNA polymerase III, anti-centromere) from available clinical laboratory testing. To facilitate comparative analysis, propensity score matching (1:1 using a greedy nearest neighbor algorithm) balanced cohorts on characteristics like age, sex, race and ethnicity, and comorbidities (Table 1). Primary outcomes included 5-year incidences of hematologic and solid-organ cancers, and varicose vein and trauma (laceration of the head) were selected as negative control outcomes. Hazard ratios (HRs) and their 95% confidence intervals (CIs) were calculated using Cox proportional hazards regressions.
Results: After propensity score matching, 66,637 patients were included in each cohort, with no statistically significant differences in baseline demographics and covariates between the treatment and control groups; in the SSc cohort, the mean age was 55.5 years (SD: 16.5) and 81.0% were female. SSc patients demonstrated elevated 5-year risks of any cancer compared to matched controls (HR 1.17; 95% CI 1.11–1.23) (Table 2). Hematologic cancer risk was significantly increased (HR 1.68; 95% CI 1.50–1.88), particularly for multiple myeloma (HR 2.13; 95% CI 1.61–2.81) and myelodysplastic syndromes (HR 2.03; 95% CI 1.49–2.77). For solid organ cancers (HR 1.23; 95% CI 1.16–1.31), esophageal cancer showed the highest risk (HR 3.96; 95% CI 2.36–6.65), followed by lung cancer (HR 2.32; 95% CI 2.00–2.69). Among autoantibody subgroups, anti-Scl-70 positive patients showed increased overall cancer risk (HR 1.40; 95% CI 1.09–1.79), RNA Polymerase III positive patients had higher rates of hematologic cancers (HR 2.56; 95% CI 1.19–5.54), while anti-centromere positive patients showed no increased cancer risks aside from a decreased melanoma risk (HR 0.26; 95% CI 0.10–0.69).
Conclusion: SSc patients demonstrate significantly increased risks for both hematologic and solid organ cancers, with risk profiles varying by autoantibody status. These findings suggest the need for targeted cancer screening strategies in SSc and further research to confirm the generalizability of these findings.
To cite this abstract in AMA style:
Mahajan A, Zangenah N, Vazquez-Machado M, LaChance A, Sparks J. Distinct Cancer Risk Profiles in Patients with Systemic Sclerosis with Autoantibody Stratification [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/distinct-cancer-risk-profiles-in-patients-with-systemic-sclerosis-with-autoantibody-stratification/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/distinct-cancer-risk-profiles-in-patients-with-systemic-sclerosis-with-autoantibody-stratification/

.jpg)
.jpg)