Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Shrinking Lung Syndrome (SLS) is a rare pulmonary complication of systemic lupus erythematosus (SLE), characterized by unexplained dyspnea, pleuritic chest pain, loss of lung volume and a restrictive ventilatory defect without overt parenchymal or pleural disease. The pathogenesis is poorly understood. Due to its rarity and non-specific presentation, the diagnosis is often delayed. Treatment is individualized, as there are no defined guidelines for management. This study aims to identify the clinical and immunological risk factors, and therapeutic interventions impacting outcome in SLS, define prognostic indicators and inform treatment management.
Methods: We compiled a pooled database of all 49 published cases of confirmed SLS associated with SLE from the literature. We then performed a retrospective analysis describing the demographic and clinical characteristics, immunological signatures and therapeutic interventions that influenced outcomes. Fisher’s exact test was used to assess the association between prognostic factors and outcomes. Odds ratio (OR) and p-values were computed.
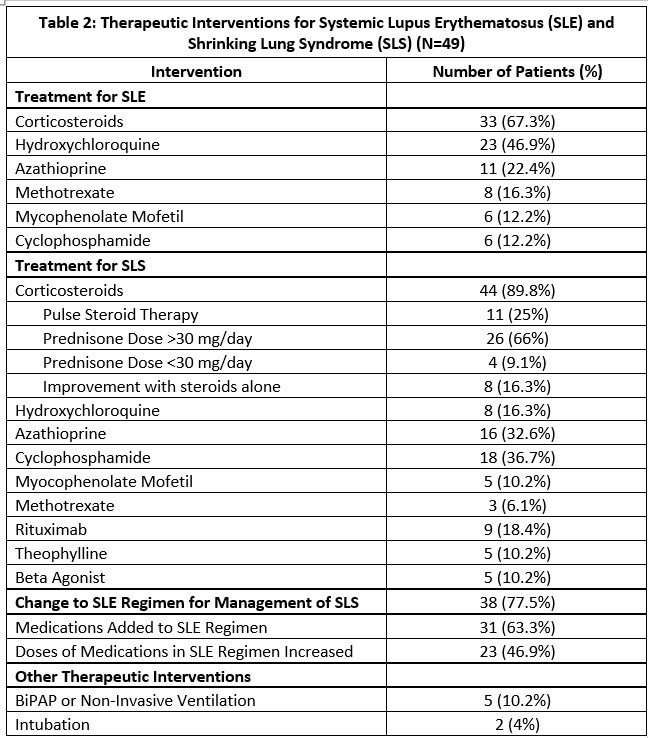
Results: The median age of SLS diagnosis was 30 years (range 12-58) and females were predominantly affected (Table 1). Median time from diagnosis of SLE to SLS was 36 months (range: 0 – 240). The most common presenting symptoms were pleuritic chest pain and exertional dyspnea (Table 1). Moderate to severe pulmonary restriction (forced vital capacity % predicted [FVCpp] < 60%) was seen in 71.4% of patients. The median nadir FVCpp was 38.5% (range 14-77). Table 2 describes the therapeutic interventions. Although improvement of symptoms with immunosuppression (corticosteroids, azathioprine, hydroxychloroquine, cyclophosphamide, methotrexate, mycophenolate mofetil [MMF], and Rituximab) was observed in 92% of patients, only 61% showed functional improvement on pulmonary function tests. Relapse or progression of symptoms were noted in 12% of patients (Table 3). Despite high morbidity, mortality was low (2%). High ANA titres ( >1:2560) (OR=33.0, p=0.027) and anti-SSA antibody positivity (OR=6.75, p=0.036) were associated with poor outcomes and these patients additionally required rituximab for management of disease. Anti-dsDNA positivity was associated with favorable outcomes, with patients demonstrating >100% increase in FVCpp after treatment (OR = 12.29, p=0.048). Anti-SSB antibody positivity (OR = 9.39, p=0.062) and the use of beta-agonists (OR = 10.02, p=0.052) were also associated with clinical and functional improvement. In contrast, treatment with azathioprine correlated with delayed symptomatic recovery exceeding 1 year (OR = 33.44, p=0.01), and MMF use was associated with increased need for non-invasive ventilation or intubation due to respiratory compromise (OR = 20.0, p=0.01).
Conclusion: SLS is a rare complication of SLE associated with high rates of morbidity. Specific immunologic profiles and therapeutic interventions were associated with better clinical and functional recovery, and can guide prognostication and treatment selection. These findings highlight the need for greater clinical awareness, and development of standardized treatment protocols to optimize patient outcomes.
 Baseline Demographics and Clinical Characteristics of Patients with Shrinking Lung Syndrome (SLS) in Systemic Lupus Erythematosus (SLE) (Nf49)
Baseline Demographics and Clinical Characteristics of Patients with Shrinking Lung Syndrome (SLS) in Systemic Lupus Erythematosus (SLE) (Nf49)
.jpg) Therapeutic Interventions for Systemic Lupus Erythematosus (SLE) and Shrinking Lung Syndrome (SLS) (Nf49)
Therapeutic Interventions for Systemic Lupus Erythematosus (SLE) and Shrinking Lung Syndrome (SLS) (Nf49)
.jpg) Outcomes of Patients with Shrinking Lung Syndrome in Systemic Lupus Erythematosus with Treatment (Nf49)
Outcomes of Patients with Shrinking Lung Syndrome in Systemic Lupus Erythematosus with Treatment (Nf49)
To cite this abstract in AMA style:
Gupta M, Raman C. Shrinking Lung Syndrome in Systemic Lupus Erythematosus: A Pooled Database Analysis of Clinical, Immunological and Therapeutic Factors Impacting Outcomes [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/shrinking-lung-syndrome-in-systemic-lupus-erythematosus-a-pooled-database-analysis-of-clinical-immunological-and-therapeutic-factors-impacting-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/shrinking-lung-syndrome-in-systemic-lupus-erythematosus-a-pooled-database-analysis-of-clinical-immunological-and-therapeutic-factors-impacting-outcomes/
