Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The ACR recommends against pregnancy in patients with SLE with high disease activity. These recommendations do not distinguish between the various manifestations of active SLE. While existing research highlights the poor outcomes associated with active LN during pregnancy, comparative data on pregnancy outcomes in patients with active non-renal SLE remain limited. This study aimed to evaluate pregnancy outcomes across different SLE disease manifestations. Given the pregnancy-related morbidity and mortality associated with social determinants of health in the U.S., this study also assessed and adjusted for characteristics of social disadvantage.
Methods: We analyzed pregnancies from prospective pregnancy registries at a U.S. center. Disease activity was assessed using the Physician’s Global Assessment (PGA) and the SLE Pregnancy Disease Activity Index (SLEPDAI). Patients were categorized into 3 groups: inactive SLE (PGA < 1.5 and SLEDAI < 6 throughout pregnancy, no renal activity), active non-renal SLE (PGA ≥1.5 in pregnancy or SLEDAI ≥6, no renal activity), and active LN (active nephritis during pregnancy). Primary outcomes included PROMISSE adverse pregnancy outcomes (APOs), severe APOs, small for gestational age, preterm birth, preeclampsia, loss after 12 weeks gestations, and APGAR score < 7 at 5 minutes. Race, education, marital status, income, and insurance were also studied. Logistic regression models estimated the association between disease activity group with pregnancy outcomes, adjusting for race and social disadvantage.
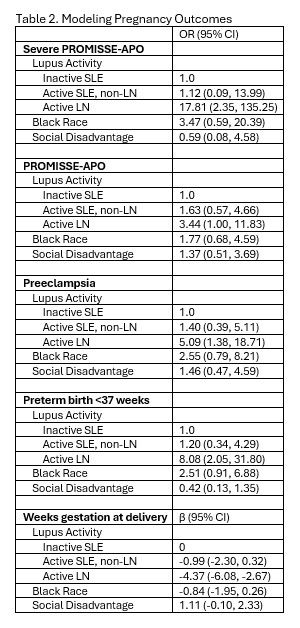
Results: We included 114 pregnancies, of which 71 patients had inactive SLE, 26 had active non-renal SLE, and 17 had active LN. Patient demographics and pregnancy outcomes are in Table 1. Nearly all patients were on HCQ (92%) and low dose ASA (87%). At least half of patients in both active SLE groups were also on AZA and prednisone. Half of patients in the LN group had active LN at their initial pregnancy visit.Active LN was associated with higher rates of APOs, including preeclampsia, preterm birth with delivery 3-5 weeks earlier, and fetal loss, compared to inactive and active non-renal SLE (Fig 1). Despite similar rates of positive dsDNA and hypocomplementemia among patients with LN and those with active non-renal SLE, patients with active non-renal SLE did not experience an increase in APOs relative to the inactive SLE group. The rates of APOs, preterm birth < 37 weeks, and preeclampsia were nearly identical between these groups.Social disadvantage was most prevalent in the active LN group (93%). In multivariate analysis (Table 2), active LN, but not race or social disadvantage, remained an independent predictor of severe APOs.
Conclusion: Active LN, but not active non-renal SLE, is a strong predictor of adverse pregnancy outcomes. While social disadvantage is associated with active LN in pregnancy, it is not an independent risk factor for adverse pregnancy outcomes. Importantly, non-renal SLE activity may not require delaying pregnancy, even in the presence of serologic activity. Our findings emphasize the need for a dual-pronged approach: prevention of pregnancy in patients with active LN and optimized management for those who conceive with active disease.
To cite this abstract in AMA style:
Trachman E, Eudy A, Clowse M. The Role of Active Nephritis, Compared to Active Non-Renal SLE, in Pregnancy Outcomes [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-role-of-active-nephritis-compared-to-active-non-renal-sle-in-pregnancy-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-role-of-active-nephritis-compared-to-active-non-renal-sle-in-pregnancy-outcomes/

.jpg)
.jpg)