Session Information
Date: Sunday, October 26, 2025
Title: (0430–0469) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Despite advancements in rheumatoid arthritis (RA) and osteoporosis management that have improved patient outcomes, osteoporosis continues to be a significant clinical concern in RA. This study aims to evaluate the effects of RA treatments and osteoporosis medications on changes in bone mineral density (BMD) over a 10-year period, using real-world longitudinal data from an RA cohort.
Methods: We conducted a retrospective analysis of RA patients enrolled in a single-center cohort at a university hospital in Japan. Patients who underwent at least two dual-energy X-ray absorptiometry (DXA) scans between 2010 and 2024 were included and followed up to 10 years. At every scan point, data on RA treatments (targeted synthetic DMARDs [tsDMARDs], biologic DMARDs [bDMARDs], methotrexate, and other conventional synthetic DMARDs [csDMARDs]) and osteoporosis medications (bisphosphonates [BPs], denosumab, vitamin D supplements, and other bone medications) were collected as time-varying exposures. BMD at the lumbar spine and femoral neck was analyzed using linear mixed-effects models to estimate the longitudinal effects of these treatments while accounting for repeated measurements and confounders.
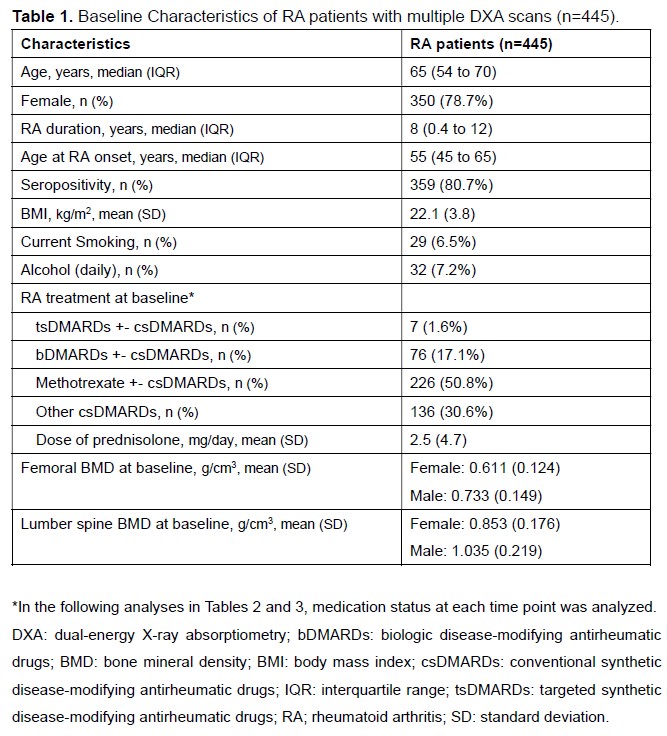
Results: We analyzed a total of 1,922 BMD measurements obtained from 445 RA patients. Baseline characteristics and clinical RA features are detailed in Table 1. At the femoral neck, treatment with tsDMARDs and bDMARDs was significantly associated with increased change rate in BMD by 7.44 (95% CI: 3.15 to 11.70) and 3.17 (95% CI: 1.00 to 5.33) mg/cm³/year, respectively, compared to csDMARDs. Among osteoporosis treatments, the use of BPs and vitamin D supplements was associated with positive BMD changes in the femur by 2.84 (95% CI: 1.15 to 4.50) and 2.05 (95% CI: 0.31 to 3.78) mg/cm³/year, respectively (Table 2). At the lumbar spine, methotrexate showed an association with increased BMD. All categories of osteoporosis medications were strongly associated with positive BMD change at the spine (Table 3).
Conclusion: This 10-year longitudinal real-world analysis underscores the protective effect of osteoporosis medications, particularly at the lumbar spine, in patients with RA. Furthermore, treatment with tsDMARDs or bDMARDs demonstrates superior efficacy in maintaining or enhancing femoral BMD compared to csDMARDs. These findings support the integration of targeted osteoporosis management alongside RA treatment strategies to mitigate bone loss in this vulnerable population.
To cite this abstract in AMA style:
Hayashi K, Hirose K, Kubota N, Terajima Y, Matsumoto K, Nakadoi T, Nawachi S, Miyawaki Y, Katsuyama E, Katsuyama T, Watanabe H, Narazaki M, Matsumoto Y, Wada J. Ten-Year Real-World Longitudinal Analysis of Bone Mineral Density in Rheumatoid Arthritis: Impact of RA and Osteoporosis Treatments [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/ten-year-real-world-longitudinal-analysis-of-bone-mineral-density-in-rheumatoid-arthritis-impact-of-ra-and-osteoporosis-treatments/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ten-year-real-world-longitudinal-analysis-of-bone-mineral-density-in-rheumatoid-arthritis-impact-of-ra-and-osteoporosis-treatments/

.jpg)
.jpg)