Session Information
Date: Sunday, October 26, 2025
Title: (0430–0469) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: In women, rheumatoid arthritis (RA) commonly presents around menopause, a timing thought to be influenced by the decline of estrogen and progesterone. However, the impact of menopausal status on disease activity and treatment response remains poorly studied. To address this, our study examined differences in baseline RA disease activity measures between pre- and post-menopausal women, as well as examining 3-month treatment response to DMARDs.
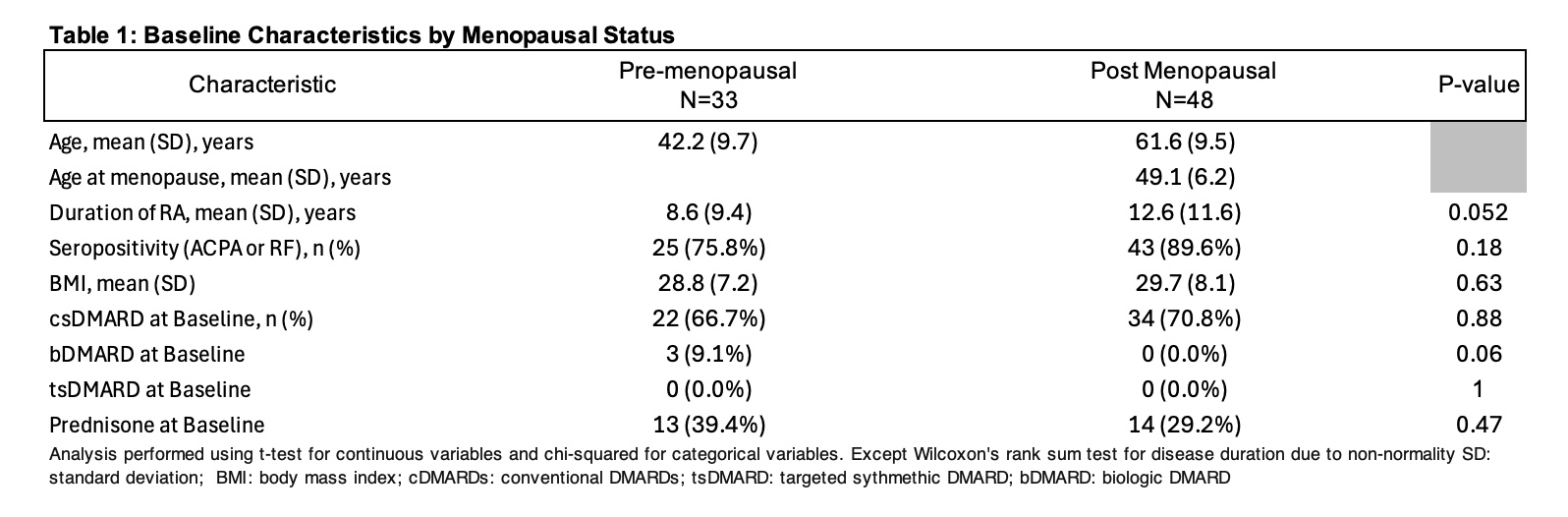
Methods: This was a retrospective study of female RA patients enrolled in one of two open-label clinical trials using tofacitinib or tocilizumab. Patients receiving oral contraceptives or hormone replacement therapy upon enrollment were excluded. Patient demographics and questionnaires were evaluated, and chart review was performed to obtain age at menopause. Patients were categorized as either pre- or post-menopausal. Post-menopausal status was defined as the absence of menses for greater than 12 months or bilateral oophorectomy. We assessed RA outcomes including composite disease activity indices (disease activity score [DAS28], clinical disease activity index [CDAI]), functional disability (health assessment questionnaire-disability index [HAQ-DI]), and musculoskeletal ultrasound (MSUS) power doppler ultrasonography (PDUS), swollen joint count (SJC28), tender joint count (TJC28), patient/physician global assessment visual analogue scales (VAS), stiffness, fatigue, and pain. Outcomes were compared between pre- and post-menopausal patients. We also compared DMARD treatment response using DAS28, CDAI, PDUS and pain at 3 months follow-up. RA duration, SJC28 and PDUS were compared with Wilcoxon’s rank sum test due to non-normality. All other continuous variables were compared with t-tests, and all categorical variables were compared with chi-squared tests. Multivariate linear regression was performed to control for potential confounding variables such as age, disease duration, and seropositivity.
Results: A total of 81 RA patients were included of whom 48 (60%) were post-menopausal. The average baseline age in the menopausal group was 62 and the average age of menopause onset was 49. Composite disease activity scores (DAS28, CDAI) and PDUS were significantly higher in the post-menopausal group (all p< 0.05. However, there were no differences between groups for functional outcomes (HAQ-DI), pain, fatigue, and stiffness. After adjusting for age, disease duration, and seropositivity, these baseline differences were no longer apparent between pre-/post-menopausal RA patients. Disease modifying anti-rheumatic drug (DMARD) treatment response at three months, assessed by DAS28, CDAI, and PDUS, did not differ between groups.
Conclusion: To our knowledge, data examining composite RA disease activity measures, PDUS, and menopausal status have not been previously reported. This study found higher baseline RA disease activity (DAS28, CDAI, PDUS) in post-menopausal women, which was no longer significant after adjusting for confounding factors. RA outcomes after 3-months of DMARD therapy were not affected by menopausal status. Our findings suggest menopausal status may not impact treatment decisions, though further research is warranted.
To cite this abstract in AMA style:
Bracamontes K, Kellner D, Chen L, Elashoff D, Brook J, Ranganath V. Menopause Status and Disease Activity in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/menopause-status-and-disease-activity-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/menopause-status-and-disease-activity-in-rheumatoid-arthritis/

.jpg)