Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Radiographs are neither sensitive nor reliable for assessing axial disease in juvenile spondyloarthritis (JSpA), though they are still used in some settings due to limited access to magnetic resonance imaging (MRI). The recently validated axial JSpA (axJSpA) classification criteria include inflammatory and structural imaging domains. When both imaging modalities are available, MRI findings are prioritized over radiographic data in the structural domain. This study evaluated the performance of the axJSpA criteria when using pelvic radiographs alone and compared these results with those based on MRI.
Methods: We conducted a retrospective analysis of an international cohort of patients with JSpA and symptom onset before age 18. All participants underwent anteroposterior (AP) pelvic radiography and dedicated pelvic MRI during axial disease evaluation. A centralized panel independently reviewed cases for unequivocal sacroiliitis: structural lesions on radiograph and both inflammatory and/or structural lesions on MRI typical of axial disease (Table 1). Imaging criteria were considered met when the majority of raters agreed. Agreement between radiograph- and MRI-defined structural lesions was assessed using Cohen’s kappa coefficient. For each subject, fulfillment of the axJSpA criteria was assessed using MRI data and radiographic data alone, in addition to non-imaging domains. For the assessment of radiographic data alone, the inflammatory lesions on imaging domain for criteria defaulted to a score of “0”.
Results: A total of 137 subjects (59.1% male; median age 14.3 years) were included. Imaging criteria were met in 40 (29.2%) cases for MRI-defined inflammatory lesions, 33 (24.1%) for MRI-defined structural lesions, and 29 (21.2%) for radiographic sacroiliitis. Agreement between MRI- and radiograph-defined structural lesions yielded a kappa coefficient of 0.54, indicating moderate concordance (Table 2). Using MRI data, 40 subjects met axJSpA classification criteria, compared to 12 using radiographic data alone. Relying on radiographic findings altered classification status in 32 (23.4%) subjects, with 2 additional cases meeting criteria and 30 cases no longer fulfilling them (Figure 1).
Conclusion: Although pelvic radiographs moderately align with MRI in identifying structural lesions, reliance on radiographic findings alone can misclassify a subset of patients under the axJSpA criteria. These findings underscore the importance of obtaining and prioritizing MRI for accurate classification and assessment of axial disease in JSpA when available. Nevertheless, in settings where MRI is unavailable, the criteria still perform reasonably when based solely on radiographic findings, supporting their utility in resource-limited contexts.
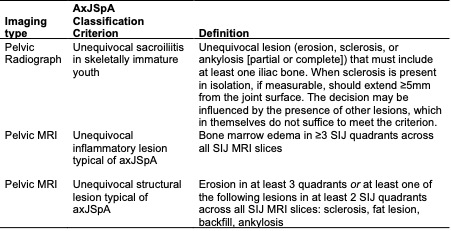 Table 1. Validated definitions for axJSpA Imaging Classification Criteria.
Table 1. Validated definitions for axJSpA Imaging Classification Criteria.
.jpg) Table 2. Agreement between radiograph- and MRI-defined structural lesions.
Table 2. Agreement between radiograph- and MRI-defined structural lesions.
.jpg) Figure 1. Re-classification of axJSpA status using MRI and radiograph as sources for imaging domain weighting. Patient classification by axJSpA status using the different imaging modality combinations were AxJSpA+ (MRI)/AxJSpA+ (Radiograph): n=10, AxJSpA+ (MRI)/AxJSpA- (Radiograph): n=30, AxJSpA- (MRI)/AxJSpA+ (Radiograph): n=2, and AxJSpA- (MRI)/AxJSpA- (Radiograph): n=95. Using radiograph-only data excluded scoring from the inflammatory lesions domain. AxJSpA+ = axial juvenile spondyloarthritis classification criteria met; AxJSpA- = axial juvenile spondyloarthritis classification criteria not met.
Figure 1. Re-classification of axJSpA status using MRI and radiograph as sources for imaging domain weighting. Patient classification by axJSpA status using the different imaging modality combinations were AxJSpA+ (MRI)/AxJSpA+ (Radiograph): n=10, AxJSpA+ (MRI)/AxJSpA- (Radiograph): n=30, AxJSpA- (MRI)/AxJSpA+ (Radiograph): n=2, and AxJSpA- (MRI)/AxJSpA- (Radiograph): n=95. Using radiograph-only data excluded scoring from the inflammatory lesions domain. AxJSpA+ = axial juvenile spondyloarthritis classification criteria met; AxJSpA- = axial juvenile spondyloarthritis classification criteria not met.
To cite this abstract in AMA style:
Biko D, Chauvin N, Francavilla M, Herregods N, Maksymowych W, Lambert R, Brandon T, Kasapcopur O, YILDIZ M, Srinivasalu H, Weiss P. Radiographic Assessment in Juvenile Spondyloarthritis: Evaluating the axJSpA Criteria Using Radiographs Alone Versus MRI [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/radiographic-assessment-in-juvenile-spondyloarthritis-evaluating-the-axjspa-criteria-using-radiographs-alone-versus-mri/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/radiographic-assessment-in-juvenile-spondyloarthritis-evaluating-the-axjspa-criteria-using-radiographs-alone-versus-mri/
