Session Information
Date: Sunday, October 26, 2025
Title: (0337–0356) Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoporosis remains underdiagnosed despite clear guidelines. As primary care physicians and trainees are key to preventive care, this quality improvement (QI) project aimed to assess provider knowledge, confidence in ordering Dual-energy X-ray absorptiometry (DEXA) scans, and perceived barriers to inform strategies for improving osteoporosis screening.
Methods: We conducted an anonymous survey with 44 physicians, including internal medicine residents (PGY-1 to PGY-3) and faculty members. The survey evaluated baseline knowledge of guidelines, perceived barriers and facilitators, and confidence in ordering DEXA scans. A knowledge score of 0-6 was calculated using the answers to questions based on guidelines. Familiarity and confidence were scored on a 3-point Likert scale. ANOVA was used for assessing statistical significance, t-tests were used for the continuous variables (confidence and familiarity scores), Chi-square tests for evaluating categorical variables (provider role vs DEXA ordering), and logistic regression was used to evaluate the predictors of ordering behaviour. Multivariate logistic regression assessed whether confidence or familiarity predicted DEXA ordering behavior. All statistical analyses were conducted in R (v4.3.2) with α = 0.05.
Results: A total of 44 providers participated in the survey, including PGY-1 (47.7%), PGY-2 (15.9%), PGY-3 (27.3%), and faculty (9.1%). Most worked in ambulatory care (56.8%) or academic hospitals (29.5%). The mean knowledge scores were high (mean = 4.95 ± 0.88), highest among faculty (5.5 ± 0.58), lowest among PGY-1s (4.00 ± 1.05), but not statistically different (ANOVA F = 0.55, p = 0.65). Participants reported being somewhat familiar with guidelines (2.36 ± 0.53) and very confident in ordering DEXA (2.51 ± 0.55).Providers who had ordered DEXA were significantly more confident (t = 7.05, p < 0.000001) and more familiar with guidelines (t = 4.51, p = 0.00005). Logistic regression showed confidence to be an independent predictor of ordering behavior (β = 3.52, p = 0.0047), while familiarity was not (β = 1.09, p = 0.405). No association was found between provider role and ordering behavior (χ² = 0.64, p = 0.42).Top barriers included lack of patient awareness (54.5%), time constraints (31.8%), and insurance issues (31.8%). Requested improvements included Electronic Health Record (EHR) based reminders (52.3%), clearer guidelines (40.9%), and improved DEXA access (40.9%). Most participants supported standardized protocols (72.7%) and integration into routine preventive care (65.9%).
Conclusion: Residents and faculty members had good awareness of osteoporosis screening, but confidence, rather than familiarity, is the strongest predictor of DEXA ordering. Providers experience both practical and systemic barriers, notably those linked to patient engagement and time. EHR reminders, clearer institutional protocols, and educational support could significantly enhance screening behavior, especially among trainees.
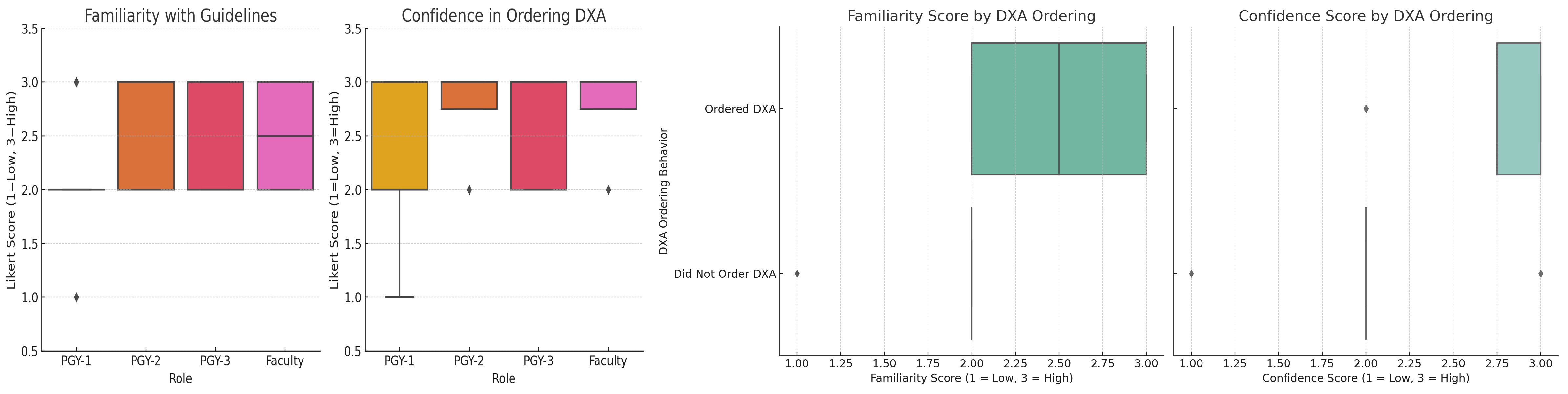 Comparison of familiarity and confidence scores by role and DXA ordering behavior; confidence was the stronger predictor of ordering; confidence was the stronger predictor of ordering behavior (p < 0.005).
Comparison of familiarity and confidence scores by role and DXA ordering behavior; confidence was the stronger predictor of ordering; confidence was the stronger predictor of ordering behavior (p < 0.005).
.jpg) Reported barriers to osteoporosis screening, stratified by DXA ordering behavior, with both groups citing time constraints and patient awareness most frequently.
Reported barriers to osteoporosis screening, stratified by DXA ordering behavior, with both groups citing time constraints and patient awareness most frequently.
.jpg) Average osteoporosis knowledge scores by role showing no statistically significant difference across PGY levels and faculty (ANOVA p = 0.65).*
Average osteoporosis knowledge scores by role showing no statistically significant difference across PGY levels and faculty (ANOVA p = 0.65).*
To cite this abstract in AMA style:
Pitliya A, Boc A, Anam H, Oletsky R, Chaudhuri D, Thirumaran R. Bridging the Bone Gap: A Quality Improvement Project on Osteoporosis Screening Practices in a Teaching Institution [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/bridging-the-bone-gap-a-quality-improvement-project-on-osteoporosis-screening-practices-in-a-teaching-institution/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bridging-the-bone-gap-a-quality-improvement-project-on-osteoporosis-screening-practices-in-a-teaching-institution/
