Session Information
Date: Sunday, October 26, 2025
Title: (0280–0305) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Fatigue significantly impacts quality of life in idiopathic inflammatory myopathies (IIM) but remains poorly understood. This study aimed to identify the key determinants of fatigue in IIM through comprehensive analysis of disease-specific, psychological, and sociodemographic factors.
Methods: Cross-sectional data from the global e-survey “Collating the Voice of people living with autoimmune diseases” were analysed. Fatigue was measured using the Visual Analogue Scale for Fatigue (VAS-F) and reported as mean±SD. Regression models were constructed to identify factors influencing fatigue across three domains: disease-associated, psychological, and sociodemographic [Fig 1 A]. Hierarchical cluster analysis using Euclidean distance and Ward’s D2 linkage was performed to identify distinct patient subgroups.
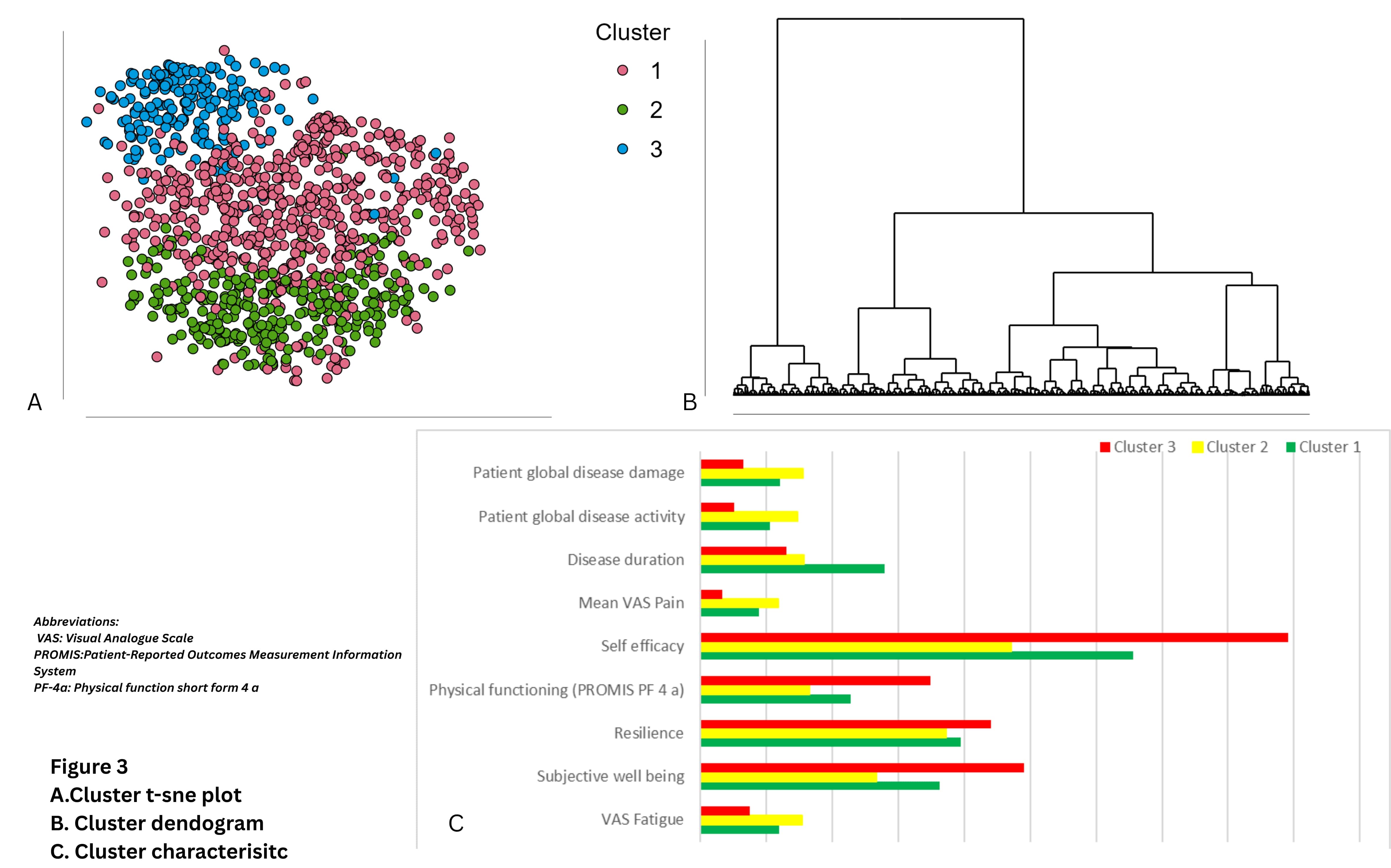
Results: Among 11,541 respondents [Fig 1 B], 1,193 (10.33%) had IIM, with fatigue significantly higher in IIM (6.04 ± 2.36) compared to healthy controls (4.11± 2.64), p< 0.001) [Fig 1 C]. Within IIM subtypes, overlap myositis (OM) reported the highest fatigue (6.63±2.29) and antisynthetase syndrome (ASyS) the lowest (5.25± 2.28) [Fig 1 D]. Disease factors explained the greatest variance in fatigue (R²=0.43), with disease activity, disease damage, pain, lung involvement, dermatomyositis (DM), inclusion body myositis (IBM), necrotizing autoimmune myositis (NAM), OM, polymyositis (PM) significantly associated with higher fatigue [Fig 2 A]. Younger age reduces fatigue risk. Among psychological factors (R²=0.31), depression, fibromyalgia, and chronic fatigue syndrome increased fatigue; while greater self-efficacy and subjective well-being were protective [Fig 2 B]. For sociodemographic variables (R²=0.19), female gender was associated with higher fatigue while non-Caucasian ethnicity, higher family functioning and household income were protective [Fig 2 C]. A composite interventional model was made where younger age, presence of basic co-morbidity, higher disease activity and damage, certain IIM subtypes (DM, NAM, OM) and high pain scores had higher fatigue scores. Shorter disease duration, higher self-efficacy, better satisfaction with life, higher resilience and non Caucasian ethnicity had lower fatigue scores [Fig.2D]. Cluster analysis [Fig 3] identified three distinct patient subgroups: Cluster 3 (predominantly DM) showed lower fatigue (3.76±2.21) and comorbidity burden, while Clusters 1 and 2 (primarily IBM, OM, and ASyS) demonstrated intermediate (6.01±2.04) and high (7.74±1.70) fatigue and disease burden, respectively.
Conclusion: Fatigue in IIM emerges as a complex multidimensional phenomenon driven by disease-specific, psychological, and sociodemographic factors. Our findings highlight the importance of integrating these domains in clinical assessment and developing targeted interventions to address fatigue in IIM patients.
A. Themes for analysis
B. Country wise respondents
C. Mean VAS Fatigue across disease group
D. Mean VAS Fatigue across IIM subtypes
A.Forrest plot showing association of disease related factors with fatigue
B. Forrest plot showing association of psychological factors with fatigue
C. Forrest plot showing association of sociodemographic factors with fatigue
D. Composite interventional model
A.Cluster t-sne plot
B. Cluster dendogram
C. Cluster characterisitc
To cite this abstract in AMA style:
Sarkar M, Shah M, Venerito V, Agarwal V, Gupta L. Multidimensional Analysis of Fatigue in Idiopathic Inflammatory Myopathies: Clinical, Psychological, and Sociodemographic Determinants [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/multidimensional-analysis-of-fatigue-in-idiopathic-inflammatory-myopathies-clinical-psychological-and-sociodemographic-determinants/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multidimensional-analysis-of-fatigue-in-idiopathic-inflammatory-myopathies-clinical-psychological-and-sociodemographic-determinants/

.jpg)
.jpg)