Session Information
Date: Sunday, October 26, 2025
Title: (0280–0305) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Idiopathic inflammatory myopathies (IIMs) are characterized by subacute onset symmetric proximal muscle weakness, with occasional extra-muscular involvement, leading to significant morbidity and mortality. Acute onset inflammatory myositis with seasonal variation has been documented1, but the role of infectious or environmental triggers in temporal clustering remains uncertain. We report on cases of acute myositis observed over a two-year period, with temporal clustering .
Methods: Records of patients admitted with acute-onset ( < 8 weeks), severe, symmetrical proximal muscle weakness between January 2023 and April 2025, unrelated to toxin exposure were reviewed and patients followed up. Demographics, clinical features, antibody profile (Euroimmun line immunoblot, 16 antigens), muscle biopsy, diagnosis, and outcomes were recorded. Patients with a dermatomyositis (DM) specific rash and/or myositis specific antibodies (MSA), perifascicular atrophy (PFA), or MXA staining on muscle biopsy were classified as dermatomyositis. Those not meeting 2016 ACR/EULAR subtypes were labeled unclassified acute myositis.Categorical data were reported as percentages, continuous as means/medians. Cox regression identified factors associated with survival and outcomes.
Results: Of 51 incident inflammatory myositis cases admitted, 33 (19 female) had acute-onset myositis, with clustering noted during September 2023–January 2024 and October–December 2024. The median (IQR) MMT-8 score was 68 (52–83). 9 patients were classified as DM. 3 of 11 non-survivors had DM and 8 unclassified acute myositis. Survivors had higher baseline MMT-8 scores and less frequent endomysial inflammation on biopsy (Table 1).Survivors were followed for a median (IQR) 61.2 (25–73) weeks. At follow-up, 4 patients were off therapy, 13 remained stable on tapering steroids or immunosuppressants, and 4 experienced flares requiring treatment escalation. Follow-up data were unavailable for 1 patient. Lower baseline MMT-8, presence of dysphagia, and MSA positivity were associated with flares or clinical worsening (Table 2).There was higher frequency of Gottron’s lesions and PFA positivity in the DM group ;prodromal symptoms and clinical improvement in the unclassified myositis group.
Conclusion: Two clusters of acute myositis observed over two years included 9 patients with dermatomyositis . There was considerable mortality which was linked to lower MMT-8 scores and endomysial inflammation . In most survivors immunosuppression was either being tapered off or stopped. Lower MMT-8, dysphagia, and MSA positivity predicted the need for escalating therapy.
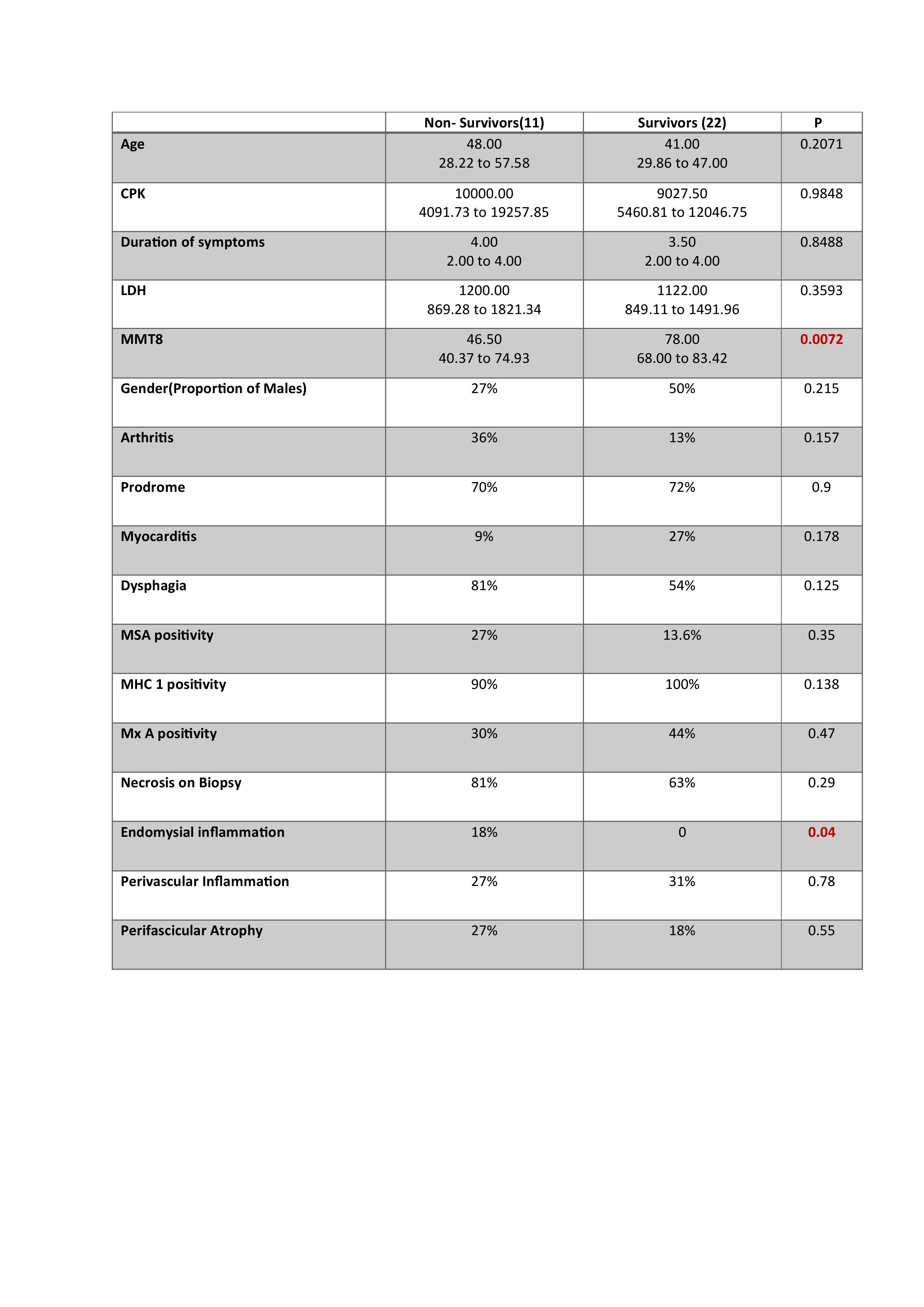 Table 1- Survivors versus Non survivors
Table 1- Survivors versus Non survivors
.jpg) Table 2- Patients with Clinical improvement versus Worsening
Table 2- Patients with Clinical improvement versus Worsening
.jpg) Figure 1- Box and Whisker Plot Depicting MMT-8 amongst various groups(0-Off all medication, 1- Tapering doses of DMARDs, 2- Tapering doses of Steroids, 3-Hiking in IS, 4- Non-Survivors
Figure 1- Box and Whisker Plot Depicting MMT-8 amongst various groups(0-Off all medication, 1- Tapering doses of DMARDs, 2- Tapering doses of Steroids, 3-Hiking in IS, 4- Non-Survivors
To cite this abstract in AMA style:
Nandita G, Challa M, D P, Gavali M, rajasekhar L. Acute onset inflammatory myositis: Clinical features and survival. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/acute-onset-inflammatory-myositis-clinical-features-and-survival/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/acute-onset-inflammatory-myositis-clinical-features-and-survival/
