Session Information
Date: Sunday, October 26, 2025
Title: (0233–0279) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Proton pump inhibitors (PPIs) are one of the most prescribed medications around the world. Recent research has increasingly identified adverse reactions in patients with long-term prescription of PPIs, including the risks of enteric infection with Clostridium difficile, osteoporosis, malignancy, ischemic stroke, myocardial infarction, and dementia. Autoimmune diseases (ADs) comprise disorders caused by an imbalance of the immune system, which leads to damage to individual tissues. The administration of medications is one of the most important factors in the induction of ADs. Some medications change the composition of the gastrointestinal microbiota, which may cause development of various diseases. Alteration of the gut microbiome can play a pathogenic role in the development of ADs.
Methods: This is a nationwide, retrospective study. We used the global, multicenter research network (TrinetX) database from 83 large healthcare organizations across multiple countries. We included patients within the age of 18-45 with a diagnosis of gastroesophageal reflux disease (GERD), or dyspepsia, from January, 2000 through September, 2024, using the International Classification of Disease-10 codes. We compared GERD, or dyspepsia patients on PPIs (Esomeprazole, Dexlansoprazole, Lansoprazole, Pantoprazole, Omeprazole, Rabeprazole, Vonoprazan), with GERD, or dyspepsia patients not on PPIs. We used 1:1 propensity score matching that accounted for demographic variables (age, gender, race); diagnoses (gastrointestinal, endocrine, nervous system, neoplastic); medication use (CNS, cardiovascular, dermatological, gastrointestinal, hormonal, musculoskeletal, genitourinary, antineoplastic agents). Index event was determined as simultaneous appearance of dyspepsia, or GERD, and PPI use in patients’ charts. Outcome of interest was the incidence of autoimmune conditions, including Sjogren’s Syndrome, Scleroderma, Rheumatoid Arthritis, Dermatomyositis, Polymyositis, SLE, Antiphospholipid Syndrome, Granulomatosis with Polyangiitis (GPA), Giant Cell Arteritis, Psoriatic Arthritis, Behcet Disease, Ankylosing Spondylitis. Patients displaying these outcomes before the index event were excluded from the analysis. Risk ratios with 95% confidence intervals were calculated for each outcome. A two-sided p-value less than 0.05 was considered statistically significant.
Results: We identified 948,767 GERD, or dyspepsia patients taking proton pump inhibitors (PPIs) and 1,427,586 patients not taking PPIs. At baseline, the mean age of diagnosis was 29.5 +8.26 years for those on PPIs and 26.9+8.96 not on PPIs. Female patients were predominant in PPI group. After propensity score matching, patients on PPIs showed higher risk of developing autoimmune conditions compared to those not using PPIs (Table 2).
Conclusion: Patients with GERD, or dyspepsia, using PPI therapy have higher risks for autoimmune disease development, compared to those patients, not on PPI therapy. Further research is warranted to elucidate the pathways through which alterations in the gut microbiota contribute to the pathogenesis of autoimmune diseases.
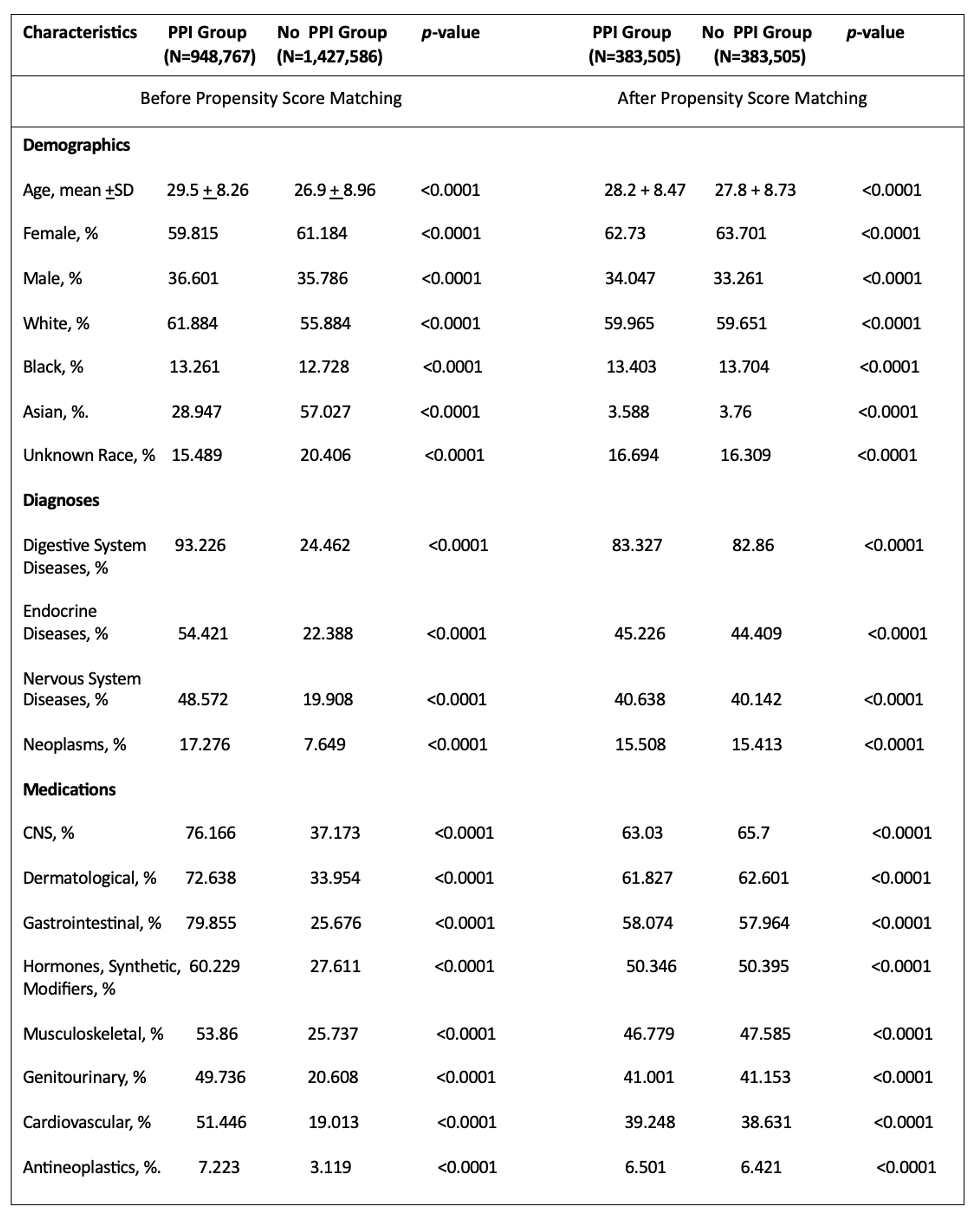 Table 1. Baseline Patient Characteristics of Study Groups, before and after Propensity Score Matching
Table 1. Baseline Patient Characteristics of Study Groups, before and after Propensity Score Matching
.jpg) Table 2. Risks of autoimmune conditions in patients (18-45) who were on chronic PPI therapy versus not on PPI therapy
Table 2. Risks of autoimmune conditions in patients (18-45) who were on chronic PPI therapy versus not on PPI therapy
.jpg) Table 2. Risks of autoimmune conditions in patients (18-45) who were on chronic PPI therapy versus not on PPI therapy (Ctd.)
Table 2. Risks of autoimmune conditions in patients (18-45) who were on chronic PPI therapy versus not on PPI therapy (Ctd.)
To cite this abstract in AMA style:
Tsibadze N, Tskhakaia I, Tskitishvili R, Rodriguez F. Chronic PPI Use Association with Development of Autoimmune Conditions: Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/chronic-ppi-use-association-with-development-of-autoimmune-conditions-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/chronic-ppi-use-association-with-development-of-autoimmune-conditions-retrospective-cohort-study/
