Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The rheumatology workforce shortage presents many challenges to the delivery of rheumatology care. Improving timely access to rheumatology for patients with life or organ threatening conditions such as SLE is one of the most important challenges. Our institution has a significant mismatch between number of referrals for new evaluation and number of new patient spots within our clinic. Further complicating the challenge of scheduling a prompt evaluation for these patients is the complex and multisystem nature of SLE. Literature suggests less than half of these referrals have inflammatory rheumatic disease (Feuchtenberger, 2016) and delays in SLE care lead to worse outcomes (Kernder, 2021). Therefore, we developed a quality improvement (QI) project to improve the time from referral to first rheumatology appointment, in this report we describe the results of our first iteration of the project.
Methods: Our study was deemed IRB exempt as a QI initiative. We implemented the Model for Improvement framework in our project (Langley, 2009). The aim statement of the project is to reduce the time from referral entry to first visit with a rheumatologist by 20% in which a diagnosis of SLE is coded. Data was collected from the medical record including ICD10 codes associated with the initial visit, date of initial visit, and date of the referral order. The first Plan, Do, Act, Study (PDSA) cycle focused on referral management. In the baseline state referrals were evaluated by a registered nurse (RN) reviewing the chart for appropriateness for rheumatology visit. That protocol did not include a mechanism to identify high risk phenotypes. Therefore, the referral process was changed to a hybrid of RN and rheumatologist review. The rheumatologist was instructed to evaluate appropriateness of referral and to risk stratify timing of the appointment. Statistical analysis was performed in R, tests of significance were Student’s T and Mann-Whitney-Wilcoxon.
Results: The first PDSA cycle was started in February of 2024, with the addition of physician review on February 19th. From October 1, 2023, to July 1, 2024, there were 4,405 referrals to rheumatology, of which 123 had a diagnosis of SLE on the first visit. The median time from referral order to first appointment was 60.5 (±59.2) days for all referrals, and 60 (±57.2) days for SLE appointments. From October 1 to February 19 the median time to appointment was 70 (±67.3) days (n 707), and from February 19 to July 31 it is 5a5 (±42.5) days (n 539) p≤0.05. For SLE appointments the median time to appointment was 69±63 days (n 73) before intervention while the time after intervention was 51±38.9 (n 50) p≤0.05. A run chart for monthly time to evaluation is included in figure 1.
Conclusion: By incorporating physician review into the referral evaluation process, we were able to decrease the time to appointment by 26% for SLE patients. Confounding our study was an expansion of our clinical faculty in January 2024 and April 2024 by 1 full time equivalent. The next iterations of our project will focus on alternative processes to further improve access for patients with high-risk disease states while reducing reliance on manual chart review. This is an area of critical need in rheumatology.
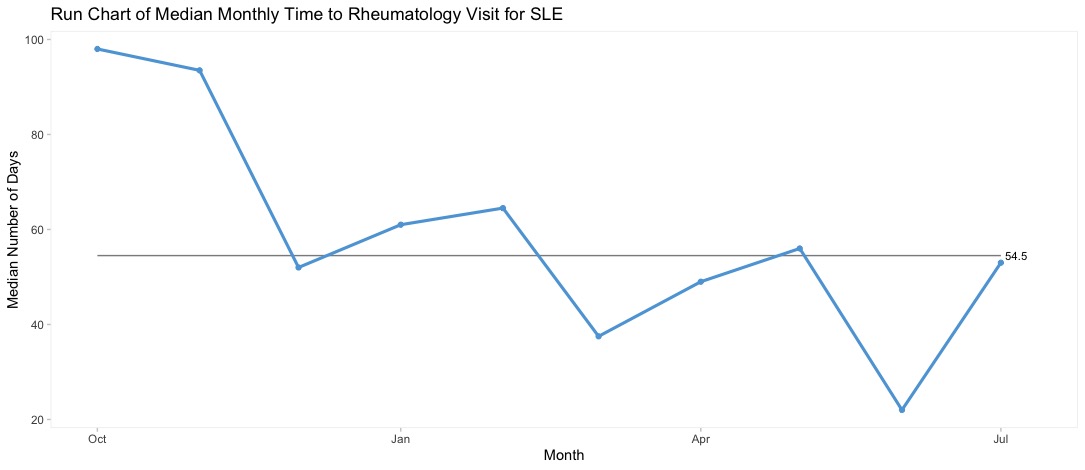 Run Chart of monthly days until rheumatology appointment for lupus patients
Run Chart of monthly days until rheumatology appointment for lupus patients
To cite this abstract in AMA style:
Taylor S, Weinstein E. Increasing Timely Rheumatology Evaluation for High Risk Lupus Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/increasing-timely-rheumatology-evaluation-for-high-risk-lupus-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increasing-timely-rheumatology-evaluation-for-high-risk-lupus-patients/
