Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Health literacy is a social determinant of health in people with chronic diseases, including inflammatory arthritis (IA). We aimed to assess the association between health literacy and comorbidity burden.
Methods: The National Early Inflammatory Arthritis Audit (NEIAA) is an observational cohort comprising adults with IA, recruited since 2018. Patients with confirmed IA, within NEIAA, were invited to complete an online survey (March to May 2024), including the Health Literacy Questionnaire (HLQ); Work Productivity and Activity Impairment questionnaire; Generalised Anxiety Disorder (GAD-2); Patient Health Questionnaire (PHQ-2); socio-demographics, employment and education; self-reported disease activity. Comorbidity data were extracted from the NEIAA for: diabetes mellitus, hypertension, lung disease, depression, and stomach ulcers.The survey was distributed to 3300 individuals with those responding matched to original records within NEIAA.Agglomerative hierarchical clustering using Ward’s method was applied. Health literacy, socio-demographics and comorbidity profile were compared between clusters.
Results: A total of 995 patients with IA were included. The median age was 59 years (IQR 50-67) and 66% were female. A five-cluster approach was deemed optimal for characterising the sample. The cohort was clustered according to normalised HLQ scores: “Highest” n=90; “High” n=190; “Moderate” n=296; “Low” n=270; “Lowest” n=149 (Figure 1 and Table 1).The “highest” health literacy cluster had highest mean age (63.4, SD 11.4), lowest proportion of females, and least likely to have ever smoked. The cluster with “lowest” health literacy had the lowest mean age (53.9, SD 11.8) and highest proportion of females (Table 1).Anxiety and depression (as measured by GAD-2 and PHQ-2) were 3.6x and 2.9x higher respectively in the “lowest” compared to “highest” health literacy cluster. Self-reported disease activity was also twice as high in the “lowest” compared to “highest” health literacy cluster.The “highest” health literacy cluster had the highest prevalence of all comorbidities, aside from diabetes, which was most frequent in the “lowest” health literacy cluster (Figure 2). The two lowest health literacy clusters had relatively high prevalence of hypertension and depression. Of the recorded comorbidities, only prevalence of hypertension and stomach ulcer were significantly different between the five clusters (p=0.02 and p=0.05 respectively).
Conclusion: The “lowest” health literacy cluster had almost four times greater anxiety and depression and twice as high self-reported disease activity, compared to the “highest” health literacy cluster. Our results suggest higher health literacy associated with older age, greater comorbidity prevalence, but lower likelihood of smoking, mental health symptoms and disease activity. Older individuals likely have more comorbidities and more frequent contact with healthcare services which may increase overall engagement and understanding of health information. Our results will inform policy and management strategies in assessing and modifying health literacy, as well as multimorbidity, in the context of IA.
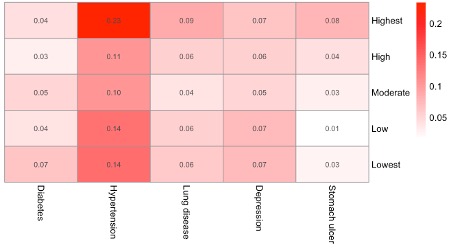 Table 1: Outcomes presented by health literacy cluster. Higher mean scores for Patient Health Questionnaire (PHQ-2) and Generalised Anxiety Disorder (GAD-2) denote higher levels of depression and anxiety, respectively. SD= standard deviation.
Table 1: Outcomes presented by health literacy cluster. Higher mean scores for Patient Health Questionnaire (PHQ-2) and Generalised Anxiety Disorder (GAD-2) denote higher levels of depression and anxiety, respectively. SD= standard deviation.
.jpg) Figure 1: Normalised Health Literacy Questionnaire (HLQ) scores by cluster (0-1 scale). The HLQ has nine domains: 1. HPS: Feeling understood and supported by healthcare providers; 2. HSI: Having sufficient information to manage health; 3. AMH: Actively managing my health; 4. SS: Social support for health; 5. CA: Appraisal of health information; 6. AE: Ability to actively engage with healthcare providers; 7. NHS: Navigating the healthcare system; 8. FHI: Ability to find good health information; 9. UHI: Understanding health information well enough to know what to do.
Figure 1: Normalised Health Literacy Questionnaire (HLQ) scores by cluster (0-1 scale). The HLQ has nine domains: 1. HPS: Feeling understood and supported by healthcare providers; 2. HSI: Having sufficient information to manage health; 3. AMH: Actively managing my health; 4. SS: Social support for health; 5. CA: Appraisal of health information; 6. AE: Ability to actively engage with healthcare providers; 7. NHS: Navigating the healthcare system; 8. FHI: Ability to find good health information; 9. UHI: Understanding health information well enough to know what to do.
.jpg) Figure 2: Mean comorbidity prevalence by health literacy cluster.
Figure 2: Mean comorbidity prevalence by health literacy cluster.
To cite this abstract in AMA style:
Dey M, Galloway J, Cope A, BUCH M, Osborne R, Norton S, Nikiphorou E. Health literacy and comorbidity burden: a cluster analysis in a national cohort of people with inflammatory arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/health-literacy-and-comorbidity-burden-a-cluster-analysis-in-a-national-cohort-of-people-with-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/health-literacy-and-comorbidity-burden-a-cluster-analysis-in-a-national-cohort-of-people-with-inflammatory-arthritis/
