Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Anti-neutrophil cytoplasmic antibodies (ANCA) associated vasculitis (AAV) includes Granulomatosis with polyangiitis (GPA), Microscopic polyarteritis (MPA) and Eosinophilic granulomatosis with polyangiitis (EGPA). Due to clinical, prognostic, and therapeutic similarities between GPA and MPA, these diseases are usually included in the same group particularly in clinical Trials. EGPA have different clinical and therapeutic features. The clinical spectrum of GPA and MPA may be quite heterogeneous, from a local limited disease to a life-threatening entity (1). Some studies reported global mortality rates ranging between 10% to almost 40%. (2,3). This wide range may be due to series including small or heterogeneous series from different hospitals and different inclusion criteria. Moreover, therapy has improved in recent years.
Our Objective was to assess the mortality and the main causes of death in GPA and MPA in a single hospital.
Methods: Observational study of patients with GPA and MPA from January 1; 2000 to December 31, 2023, in a single University Hospital in Northern Spain. AAV were classified accordingly to EULAR/ACR 2022 criteria. Person-year (PY) at risk was calculated for each patient as time from the date of diagnosis through the date of death. Mortality rates were expressed as cases by 106 habitants per year (95% IC) and the Case Fatality rate expressed as percentage (95% IC), the accumulative incidence of mortality was expressed in cases by 103 PY. The population data were obtained from the Regional Health Service’s annual reports. We consider 2 groups of GPA and MPA: a) study group (dead patients) and b) Control group (remaining patients).
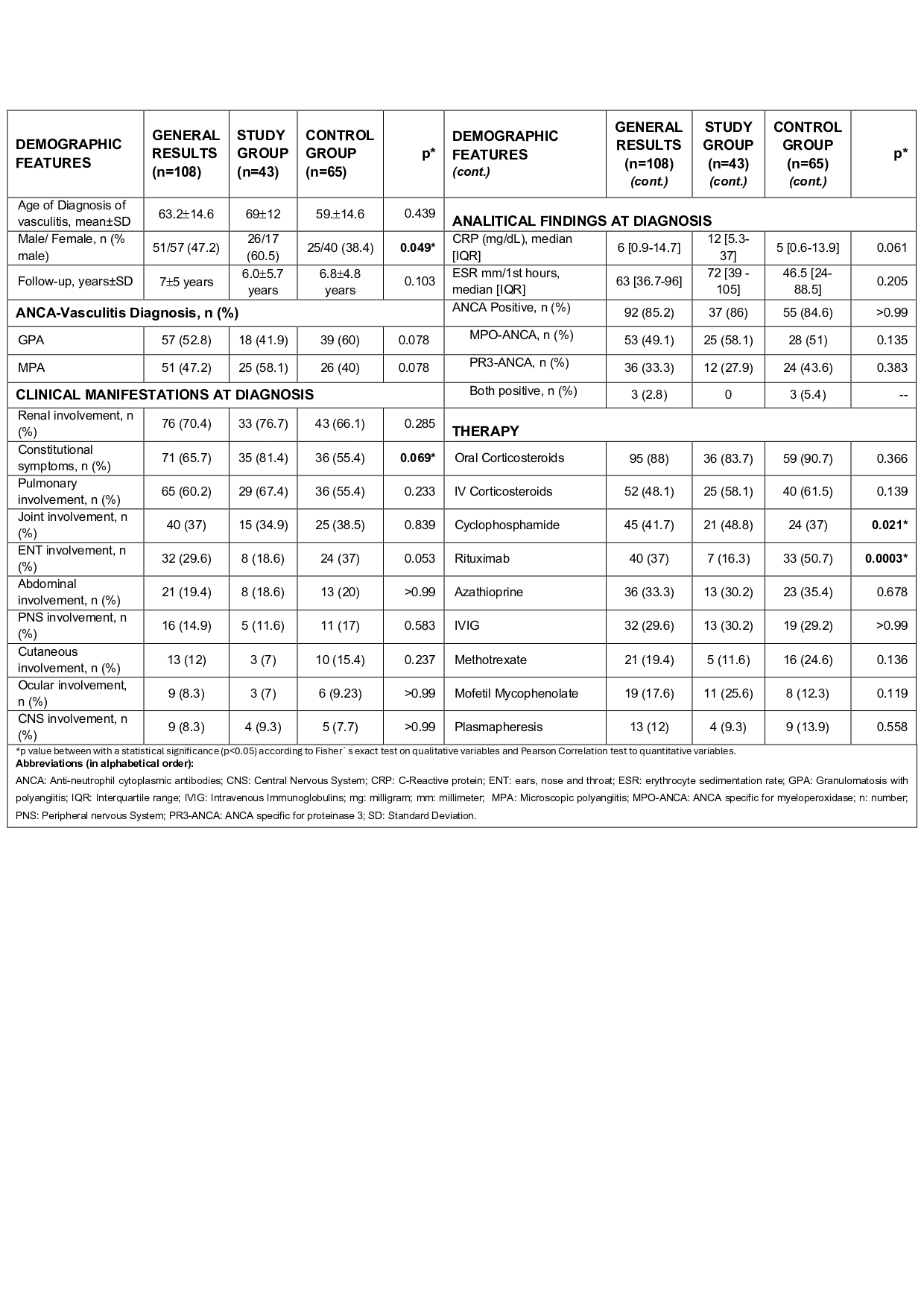
Results: We studied 108 patients, mean age 63.2±14.6 years with 709 person-year (PY) (57 GPA; 52.8%)/51 MPA; 47.2%). Death was observed in 43 of 108 cases (39.8%), (study group). The General Mortality rate was 3.8/106 habitants per year (95% IC: 2.4-5.1). The case fatality rate was 41% (95% IC: 27.2-54.7). The accumulative incidence of death was 60.6/103/PY (95% IC: 60-61.2).
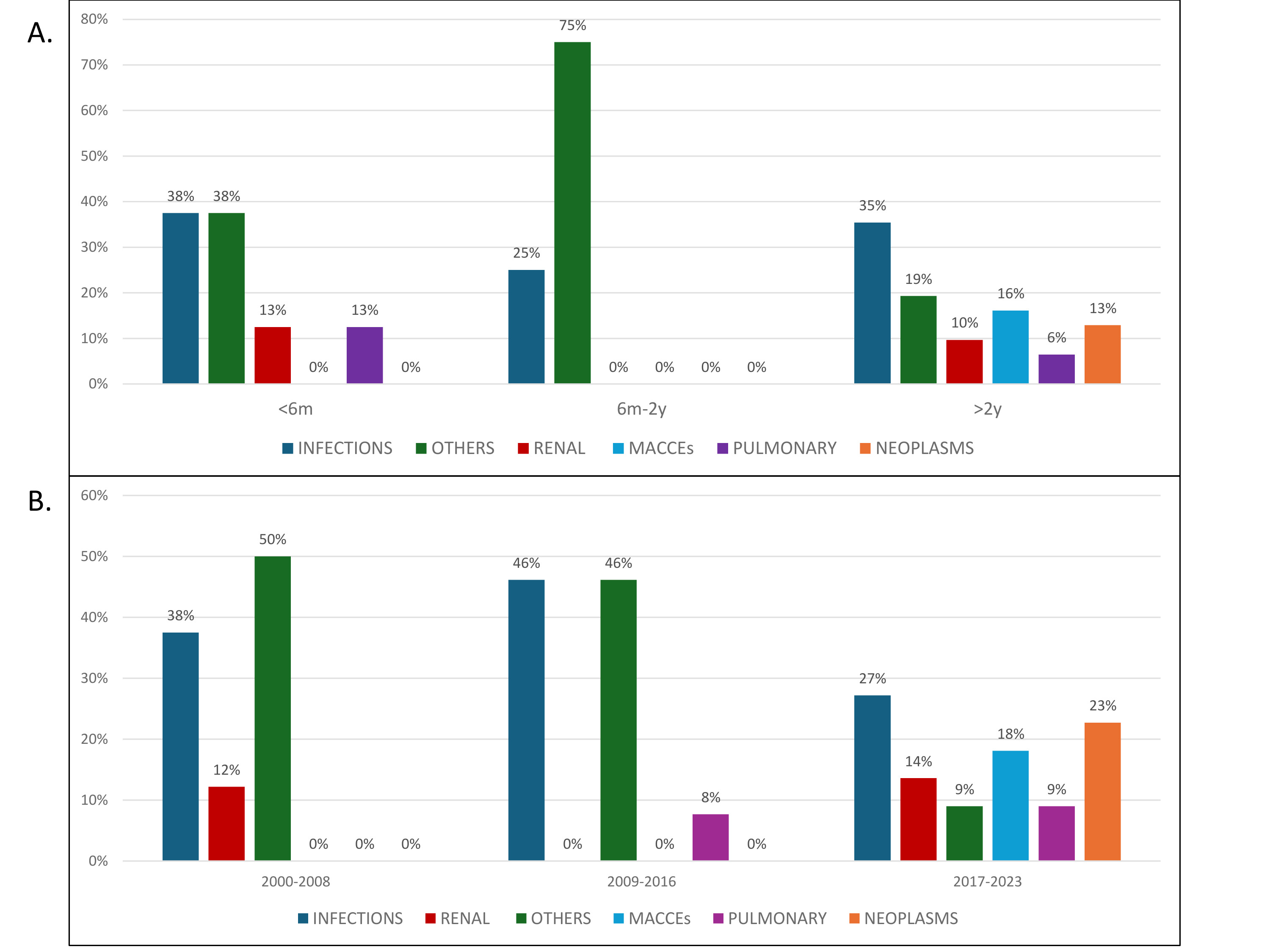
The main causes of death were infections (n=15; 34.9%), Major adverse cardiovascular events (MACE) (n=5; 11.6%), neoplasia, (n=4; 9.3%), renal complication (n=4; 9.3%) and pulmonary complications without infections (3n=3; 6.9%).
Death was more frequent after 2 years (71.8%). (FIGURE A). Infections were the most frequent cause of death (15 patients, 34.9%) on early (< 6 months), late ( > years) and at any time (2000-2008, 2017-2023) (FIGURE B). As expected, neoplasms appear in long term follow-up (9.3%).
The study group (dead patients) compared with control group show a non-significant more frequent MPA, constitutional symptoms, pulmonary and renal involvement at time of diagnosis (TABLE).
Conclusion: Mortality rates, the Case Fatality rate and the accumulative incidence of mortality in GPA and PAM remains relatively high. Infections are the most frequent cause followed by MACE.
To cite this abstract in AMA style:
Benavides F, Herrero-Morant A, Prieto-Peña D, Calvo-Rio V, Al Fazazi S, Martín-Gutiérrez A, Renuncio-García M, Sánchez-López A, Poo-fernandez C, Escagedo-Cagigas C, Rodríguez-Vidriales M, Blanco-Alonso R. Mortality in Anti-neutrophil Cytoplasmic Antibody-Associated Vasculitis: Study from a Single University Hospital [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/mortality-in-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis-study-from-a-single-university-hospital/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mortality-in-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis-study-from-a-single-university-hospital/