Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Endogenous estrogens (E) appear cardioprotective in women in the general population. Yet, proinflammatory effects were described in chronic autoimmune diseases depending on stage, cell-type involved, target organ environment and their metabolism. The impact of E on coronary atherosclerosis and cardiovascular (CV) risk in rheumatoid arthritis (RA) is unknown. We here explored the association between serum E, coronary atherosclerosis and CV risk in patients with RA.
Methods: Atherosclerosis (noncalcified, mixed or fully calcified, and low-attenuation plaque) was evaluated with computed tomography angiography in 140 patients without CV disease and reassessed in 100 after 6.9±0.4 years. Lesions with >50% stenosis were considered obstructive. Bioactive estrone (E1) and 17β-estradiol (E2) were measured at baseline and follow-up with ELISA. Multivariable robust negative binomial regression evaluated interactions of E with age and ACPAs predicting plaque numbers at baseline, and interactions of E with time-averaged C-reactive protein (TA-CRP) predicting numbers of new plaques. Multivariable Cox regression evaluated the association of E with CV risk. All models minimally adjusted for atherosclerotic CV disease (ASCVD) score while plaque progression and CV risk models further adjusted for baseline plaque.
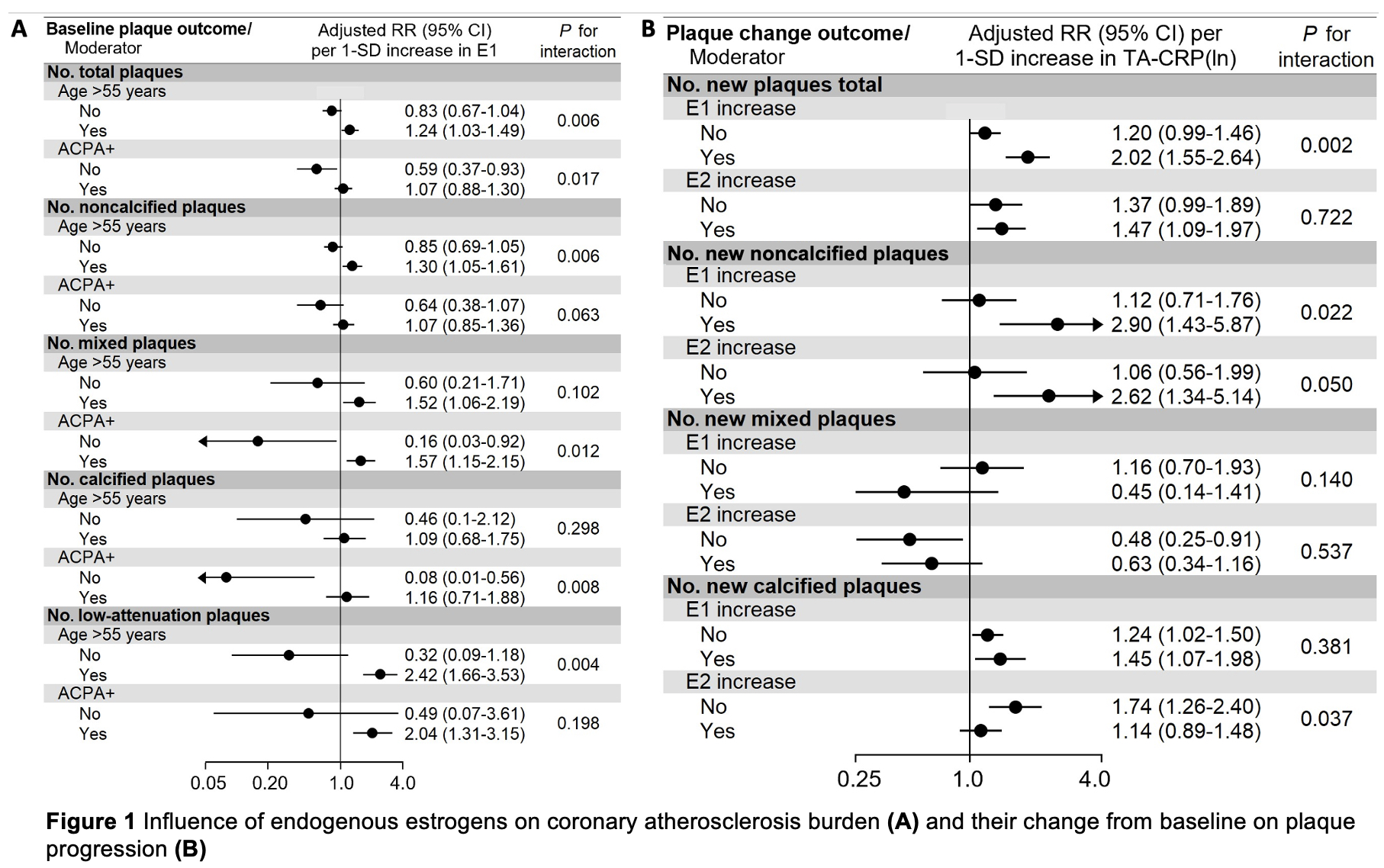
Results: E1 associated with total plaque burden, noncalcified and low-attenuation plaques in patients older than 55 (p-interaction = 0.006, 0.006 and 0.004, Figure 1A). Higher E1 associated with fewer total, mixed and fully calcified plaques in ACPA negative (p-interaction = 0.017, 0.012 and 0.008) and more mixed plaques in ACPA positive patients (Figure 1A). The interactions of E2 with age > 55 years and ACPA status were not significant (not shown). In patients with increasing -but not decreasing- E1, higher TA-CRP(ln) associated with new total and noncalcified plaques (p-interaction = 0.002 and 0.022, Figure 1B). Likewise, higher TA-CRP(ln) associated with new noncalcified lesions only in patients with increasing E2 (p-interaction = 0.050); in contrast, in those with decreasing E2, higher TA-CRP associated with new fully calcified (low-risk) lesions (p-interaction = 0.037, Figure 1B).
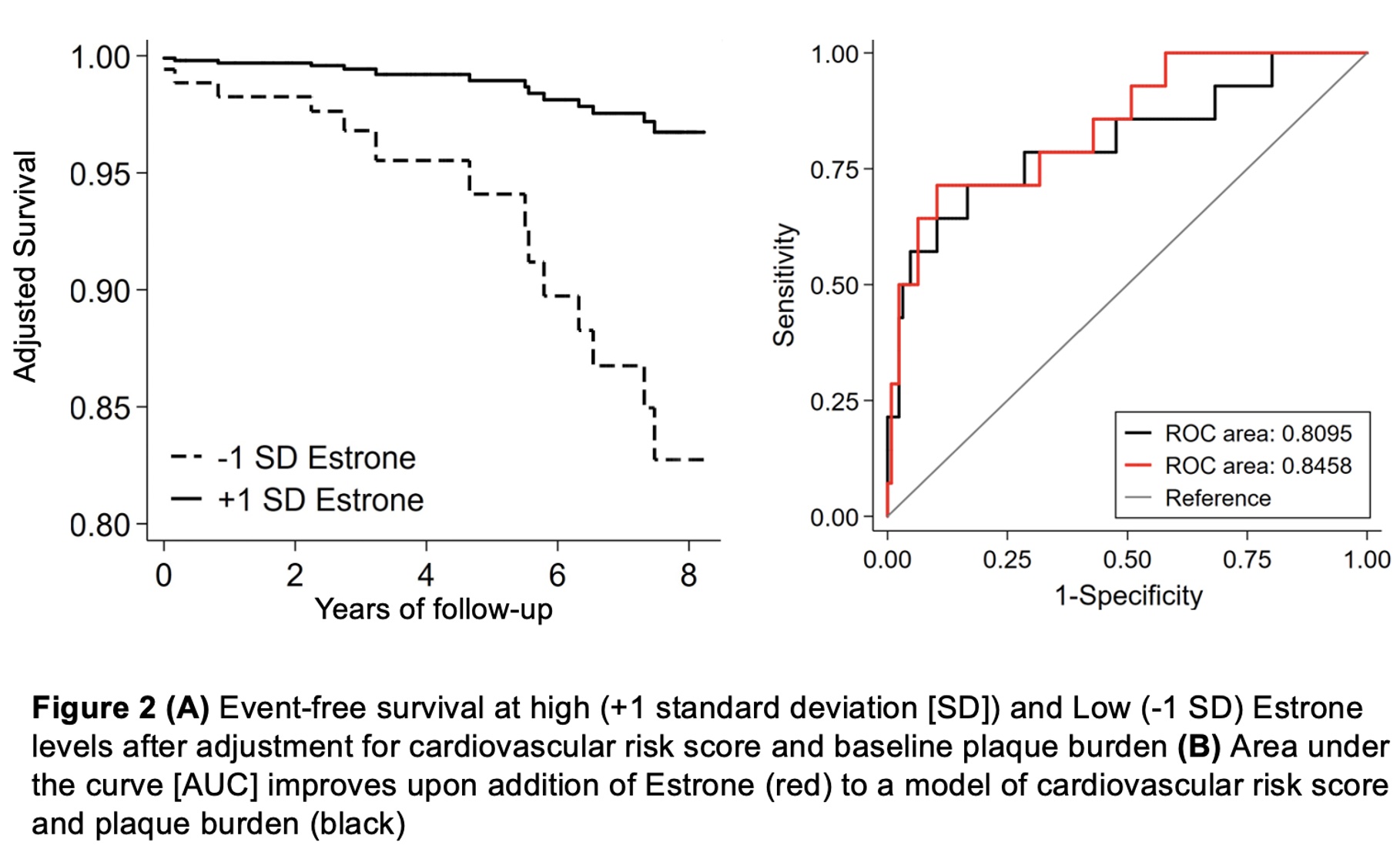
E1 inversely associated with CV risk (adjusted hazard ratio- aHR 0.39, 95% confidence interval- CI 0.19-0.81 per standard deviation-SD increase in E1, Figure 2A) while E2(ln) did not (HR 0.87, 95% CI 0.50-1.51 per SD increase). Addition of E1 to ASCVD and baseline plaque enhanced CV risk prediction; area under the curve (AUC) increased from 0.81 (95% CI 0.66-0.95) to 0.85 (95% CI 0.73-0.96) and integrated discrimination improvement (IDI) = 0.06 (standard error 0.023), p = 0.008 (Figure 2B). The inverse association of E1 with CV risk was stronger in patients < 55 (HR 0.17, 95% CI 0.06-0.48) and those without obstructive plaque (HR 0.21, 95% CI 0.09-0.48, p-interaction = 0.008 and 0.002).
Conclusion: Conclusion: Effects of E on atherosclerosis vary according to age and ACPA status, and their increase over time yielded a stronger association between cumulative inflammation and plaque progression. E1 inversely associated with CV risk, suggesting additional benefits of E on plaque biology and stability.
To cite this abstract in AMA style:
Karpouzas G, Papotti B, Ormseth S, Palumbo M, Hernandez E, Budoff M, Ronda N. Age, Seropositivity and Inflammation Determine Risk versus Benefit of Endogenous Estrogens on Coronary Atherosclerosis in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/age-seropositivity-and-inflammation-determine-risk-versus-benefit-of-endogenous-estrogens-on-coronary-atherosclerosis-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/age-seropositivity-and-inflammation-determine-risk-versus-benefit-of-endogenous-estrogens-on-coronary-atherosclerosis-in-rheumatoid-arthritis/