Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: VEXAS (Vacuoles, E1 enzyme, X-linked, Autoinflammatory, Somatic) syndrome, first described in 2020, is an autoinflammatory condition characterized by somatic mutations in the UBA1 gene. Predominantly affecting elderly males, VEXAS syndrome manifests with systemic inflammation and refractory hematologic abnormalities. Despite advancements in our understanding of this condition over the last 4 years, treatment recommendations for VEXAS syndrome are lacking. We analyzed individual case reports and case series published between October 2020 and January 2024 with the aim of identifying effective treatments options for this complex and often fatal condition.
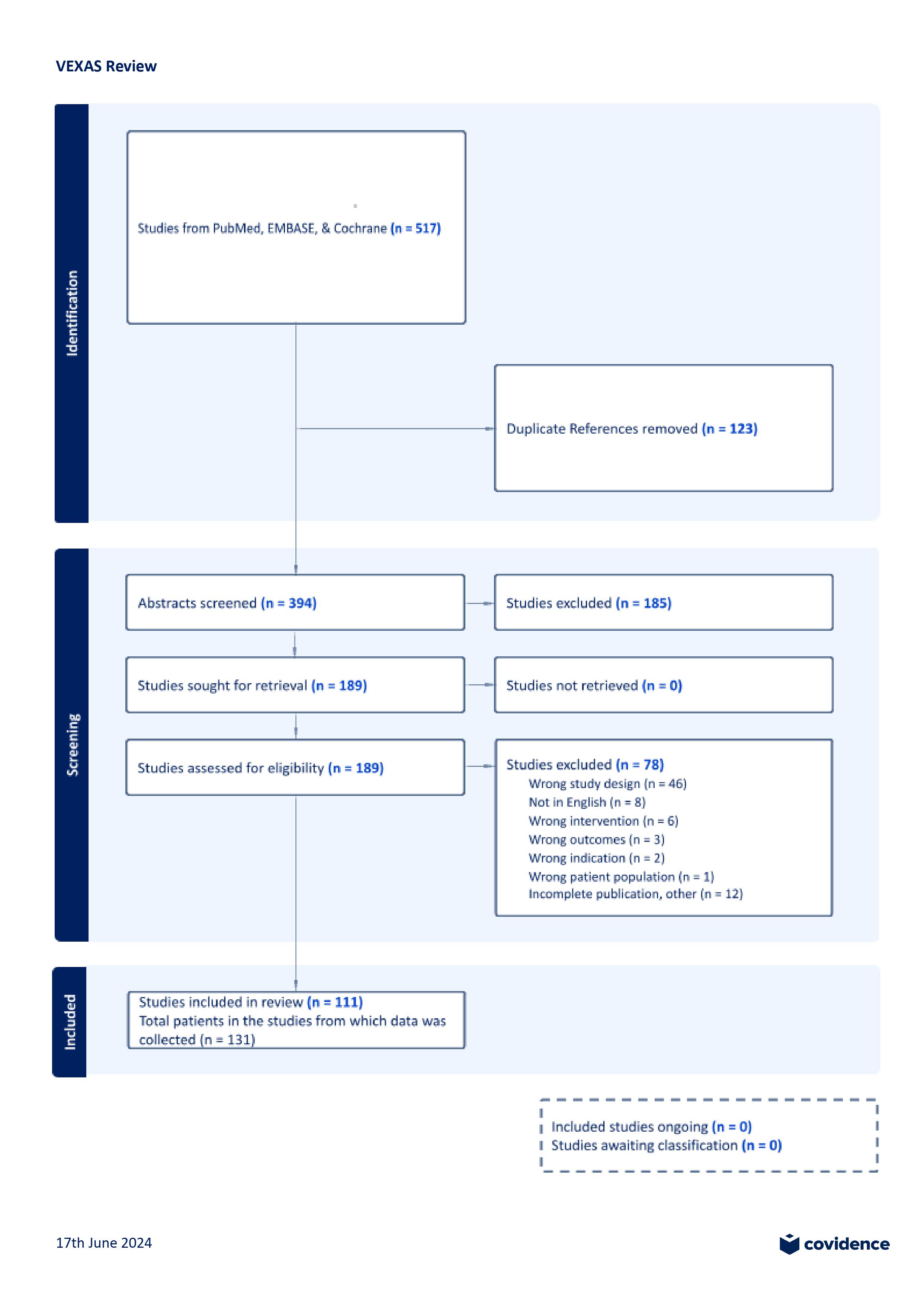
Methods: We conducted a comprehensive literature review using major databases, including PubMed, EMBASE, and Cochrane Library, focusing on articles that mentioned “VEXAS” and “treatment.” The initial search identified 517 articles (figure 1). After removing 123 duplicates, 394 unique articles remained. Of these, 185 were excluded due to the absence of clear treatment mentions. The remaining 189 articles were further screened based on study design, language, interventions, outcomes, and patient population. Eligible study designs included case studies, case series, and cohort studies. Twelve articles were excluded due to insufficient information, leaving 111 articles for inclusion in the review. From these, we gathered data on a total of 131 individual patients and the treatments implemented. We grouped treatment responses into four categories: complete response (CR), partial response (PR, with or without glucocorticoids), no response, and/or death (NR/D).
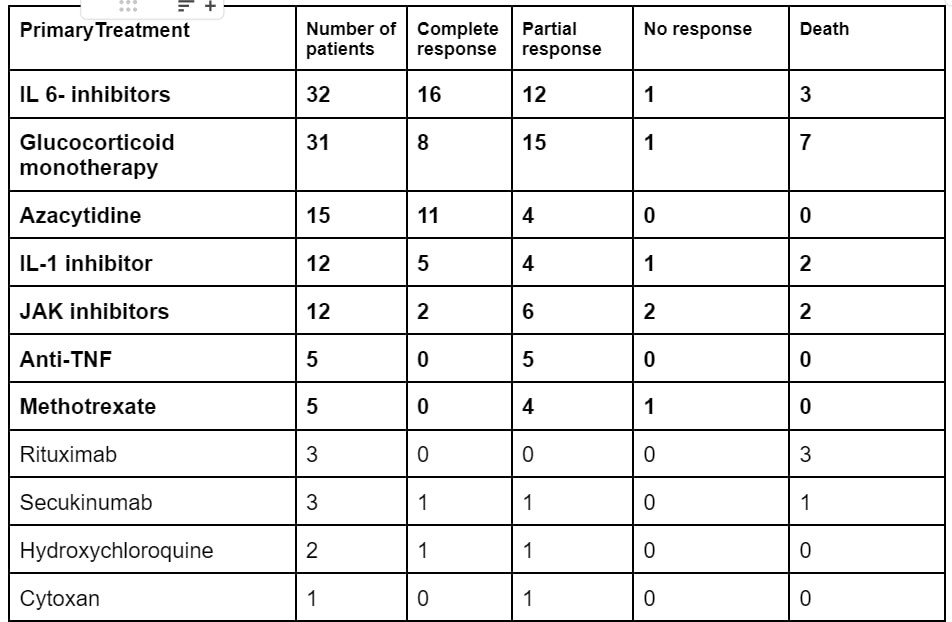
Results: We identified 111 publications with a total of 131 individual patients (table 1), of which 129 were male, with an average age of 67.5 yrs. Primary treatments included IL-6 inhibitors (32 patients: CR 50%, PR 37.5%, NR/D 12.5%), Azacytidine (15 patients: CR 73.3%, PR 26.6%, NR/D 0%), IL-1 inhibitors (12 patients: CR 41.6%, PR 33.3%, NR/D 24.9%), JAK inhibitors (12 patients: CR 16.6%, PR 50%, NR/D 33.2%), glucocorticoid monotherapy (31 patients: CR 25.8%, PR 48.3%, NR/D 25.8%), methotrexate (5 patients: CR 0%, PR 80%, NR/D 20%), and anti-TNF therapy (5 patients: CR 0%, PR 100%, NR/D 0%). Less than five individual reports were available for rituximab, sekukinumab, abatacept, hydroxychloroquine, and cytoxan. Data on adverse events were available for 32 patients and included worsening cytopenias, infections (including herpes zoster, pneumonia, and diverticulitis), and side effects related to chronic steroid use.
Conclusion: VEXAS syndrome remains a challenging condition to manage, with no clear consensus on the optimal treatment approach. The most common treatments tried in VEXAS include IL-6 inhibitors, IL-1 inhibitors, JAK inhibitors, azacytidine, and glucocorticoid monotherapy. Most patients required co-administration of glucocorticoids (more than 10 mg of prednisone) to help manage their disease activity. Glucocorticoid monotherapy, however, was generally less efficacious than the monotherapies and associated with more side effects.
To cite this abstract in AMA style:
Vijaya Prakash A, Garcia J, Goel A, Gilvaz V, Midha R. A Systematic Review of Treatment Strategies in VEXAS Syndrome [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/a-systematic-review-of-treatment-strategies-in-vexas-syndrome/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-systematic-review-of-treatment-strategies-in-vexas-syndrome/