Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with SLE arthritis face chronic, disabling symptoms, and progressive joint damage. Arthritis/arthralgias is one of the most common symptoms of lupus. The heterogeneity of lupus arthritis and the shortcomings of arthritis measurements contribute to diagnostic/treatment delays and clinical trial failures. In a preliminary study, with 20 lupus patients and 10 healthy volunteers, we showed that optical tomographic imaging (OTI) can differentiate inflamed SLE joints from normal joints. We are able to determine the spatial distribution of physiologically relevant tissue parameters by shining a near-infrared light onto joints and measuring transmitted and reflected light intensities.
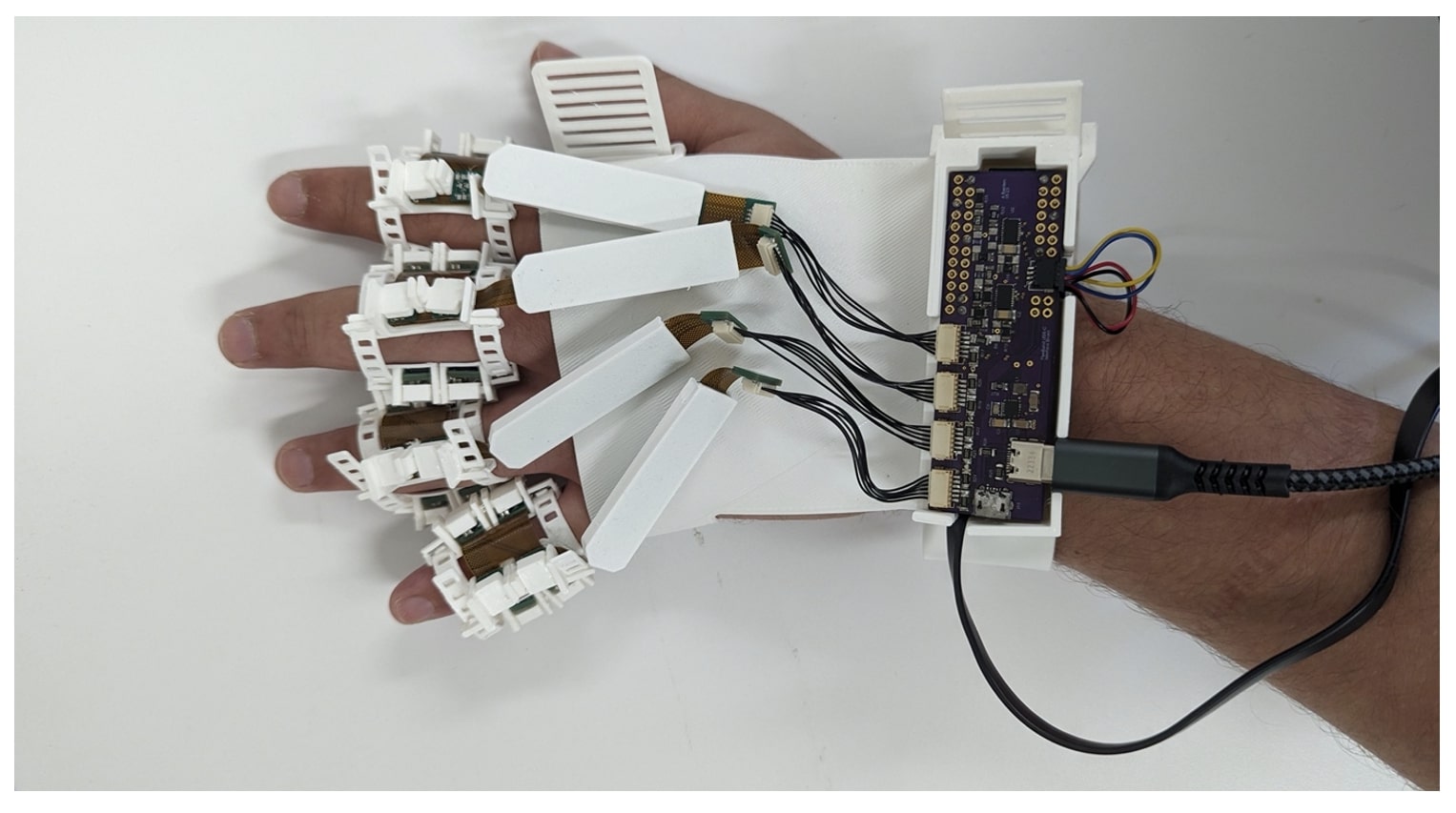
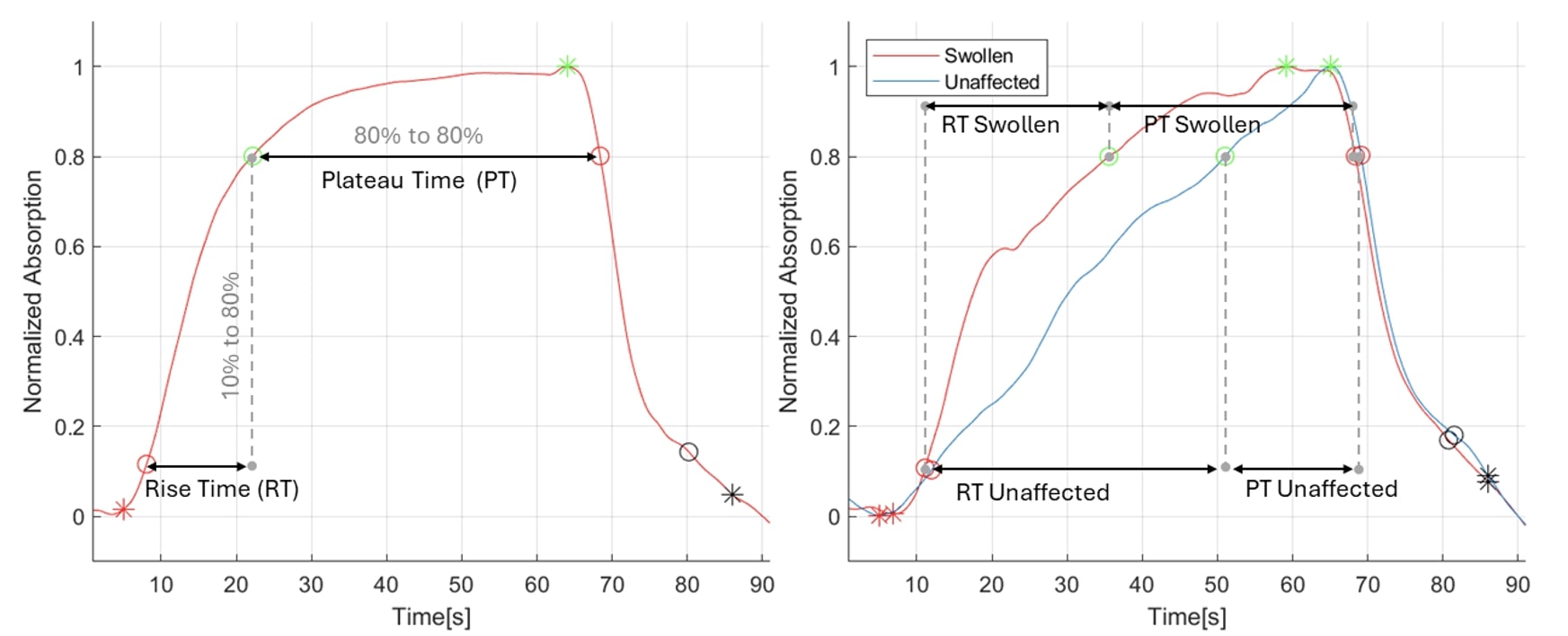
Methods: We designed and evaluated a glove-like optical imaging system (GLOIS) to measure lupus arthritis, figure 1. The optical instrumentation utilized flexible bands with eight optical modules wrapped around the joints. Each module contained a photodiode and three light-emitting diodes (LEDs) (wavelengths λ=530 nm, 660 nm, and 880 nm). The LEDs were lit sequentially, and the photodiodes captured the corresponding readings. Twelve SLE patients were evaluated. Each patient had up to 8 proximal interphalangeal (PIP) joints (bilateral PIP 2-5) imaged using the optical imaging system, resulting in 67 joint images. Physician evaluations determined tender and swollen joints; painful joints are based on patient-report. The hemodynamic effect was obtained using a BP cuff; after a 30s baseline measurement, the BP cuff was inflated to the subject’s diastolic blood pressure (DBP) and kept inflated for 1 minute while optical image measurements were obtained. A second measurement was recorded at the subject’s mean arterial pressure (MAP). We acquired the rise-time (RT) and plateau-time (PT) from the recorded hemodynamic response for each wavelength at each pressure point. Figure 2 represents optical changes associated with hemodynamic response and illustrates the RT and PT.
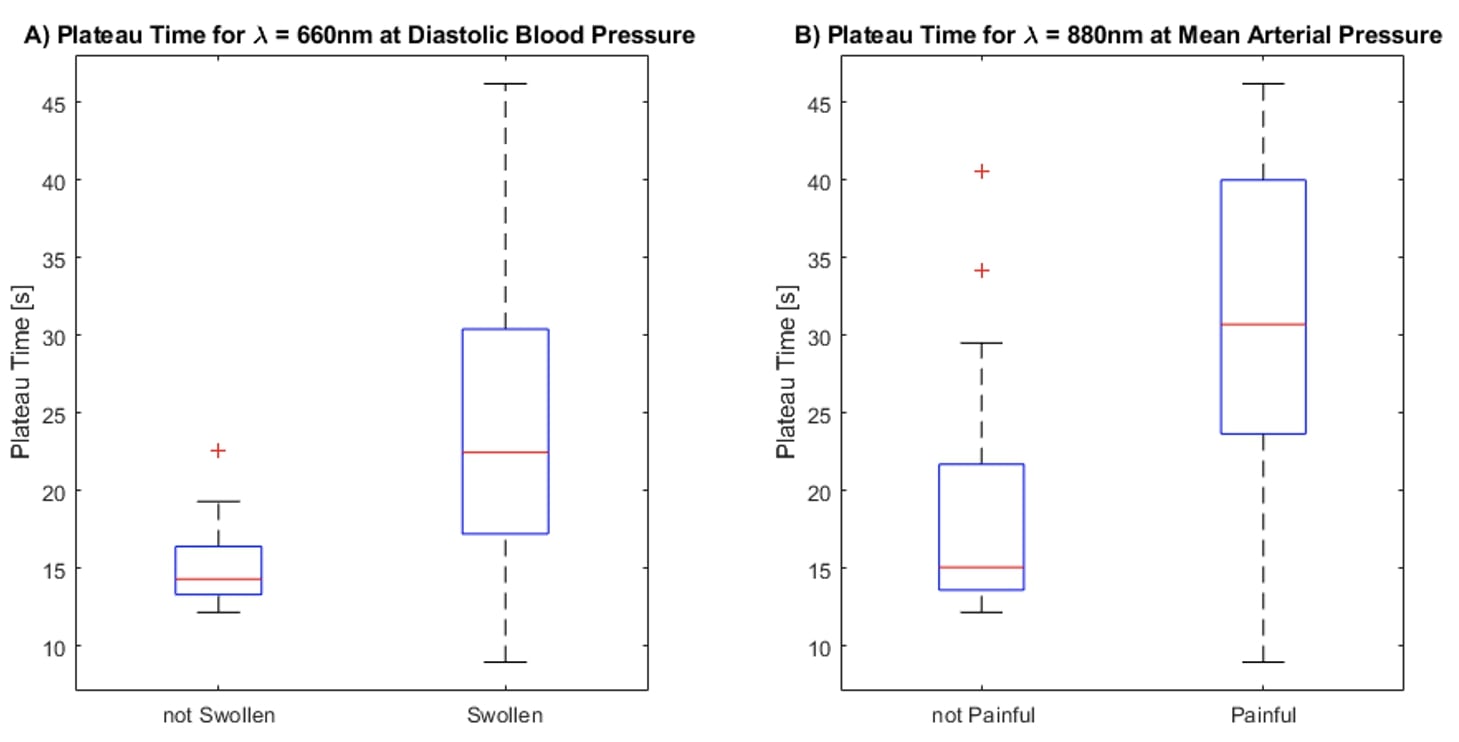
Results: Out of the 67 joints evaluated 52 were swollen, 19 tender, and 15 painful. Optical measurements of hemodynamic responses and swollen joints were best correlated at 660nm, DBP, and PT (ρ =0.47, p< 0.001); the mean PT for unaffected and affected joints were 15.3+/-2.9s and 23.9+/-9.3s. Optical measurements of hemodynamic responses and painful joints were best correlated at 880nm, MAP, and PT (ρ =0.61, p< 0.001); the mean PT for unaffected and affected joints were 19.1+/-8.7s and 30.8+/-10.8. Figure 2 shows a box plot showing the differences between PT in affected and unaffected joints for the correlations presented. Tenderness did not correlate with optical tracings.
Conclusion: These data show that swollen and painful fingers have different hemodynamic responses compared to unaffected fingers. Tenderness did not correlate with optical changes. OT has the potential to provide the much-needed objective data in the assessment of lupus arthritis to improve arthritis evaluations in clinical care and clinical trials. Further development of this technology is currently underway and necessary.
To cite this abstract in AMA style:
Tang W, Khalili L, Bardien M, Marone A, Gong C, Wang X, Murray S, Kim S, Hielscher A, Geraldino L, Askanase A. Comparison of a Dynamic Optical System with Physician Physical Assessment of PIP Joints of Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/comparison-of-a-dynamic-optical-system-with-physician-physical-assessment-of-pip-joints-of-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-a-dynamic-optical-system-with-physician-physical-assessment-of-pip-joints-of-systemic-lupus-erythematosus-patients/