Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Social determinants of health (SDoH) may impact health outcomes via neighborhood-level factors, such as access to medical care and neighborhood safety. Therefore, geocoded measures of neighborhood social deprivation, such as Area Deprivation Index (ADI) and Childhood Opportunity Index (COI), may be important to understand health disparities affecting children with rheumatic disease. Our primary aim was to assess the association between neighborhood deprivation (via ADI and COI) on emergency department (ED) use and inpatient hospitalization among youth seen frequently in pediatric rheumatology clinic. We hypothesized that higher levels of neighborhood deprivation would be associated with increased ED use and inpatient hospitalization.
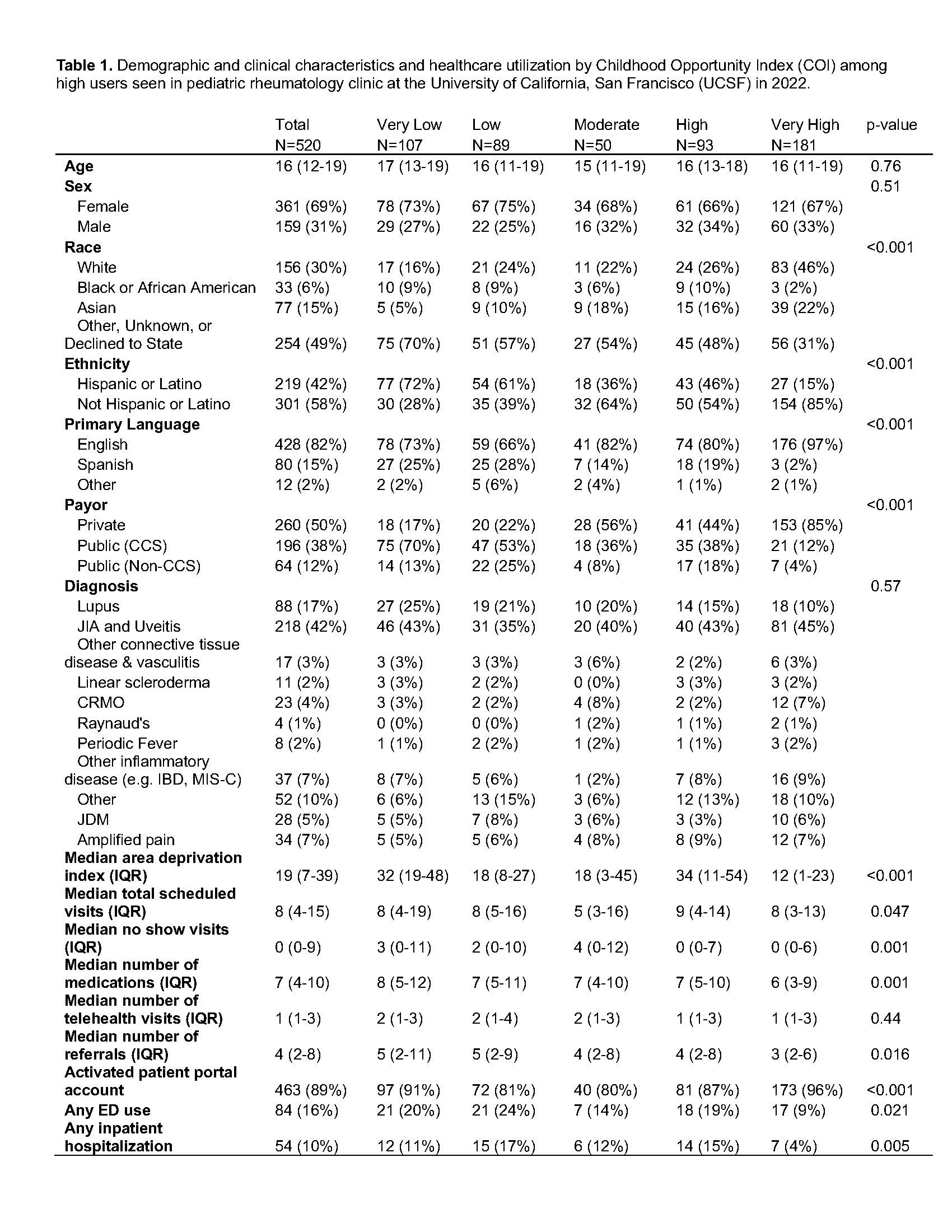
Methods: Subjects defined as frequent presenters to pediatric rheumatology clinic at the University of California, San Francisco (UCSF) were identified between 1/1/2022-12/31/2022 by the presence of at least 6 healthcare encounters over the preceding 3-year period with a primary subspecialty clinic in rheumatology. The primary predictor variables were 1) ADI geocoded to 9-digit ZIP code and 2) COI geocoded to 5-digit ZIP code. The outcome variables were 1) any emergency department use and 2) any inpatient hospitalization. Descriptive statistics were performed to describe the cohort by COI using Kruskal Wallis and chi-squared tests, as appropriate. Univariate and multivariable (age, sex, primary diagnosis, race, ethnicity, primary payor, primary language, distance to care, site of care) logistic regression models were created to investigate the association between our predictor and outcome variables.
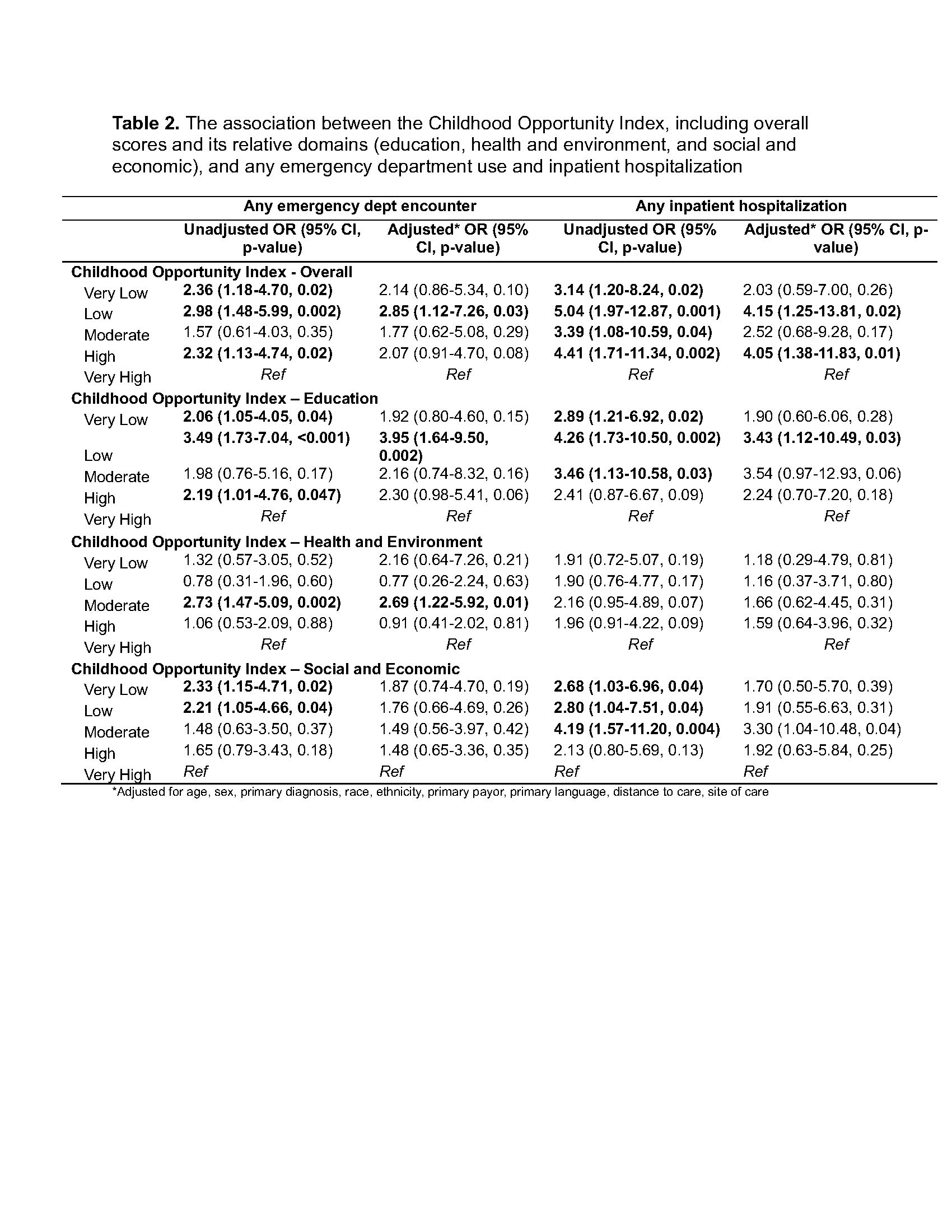
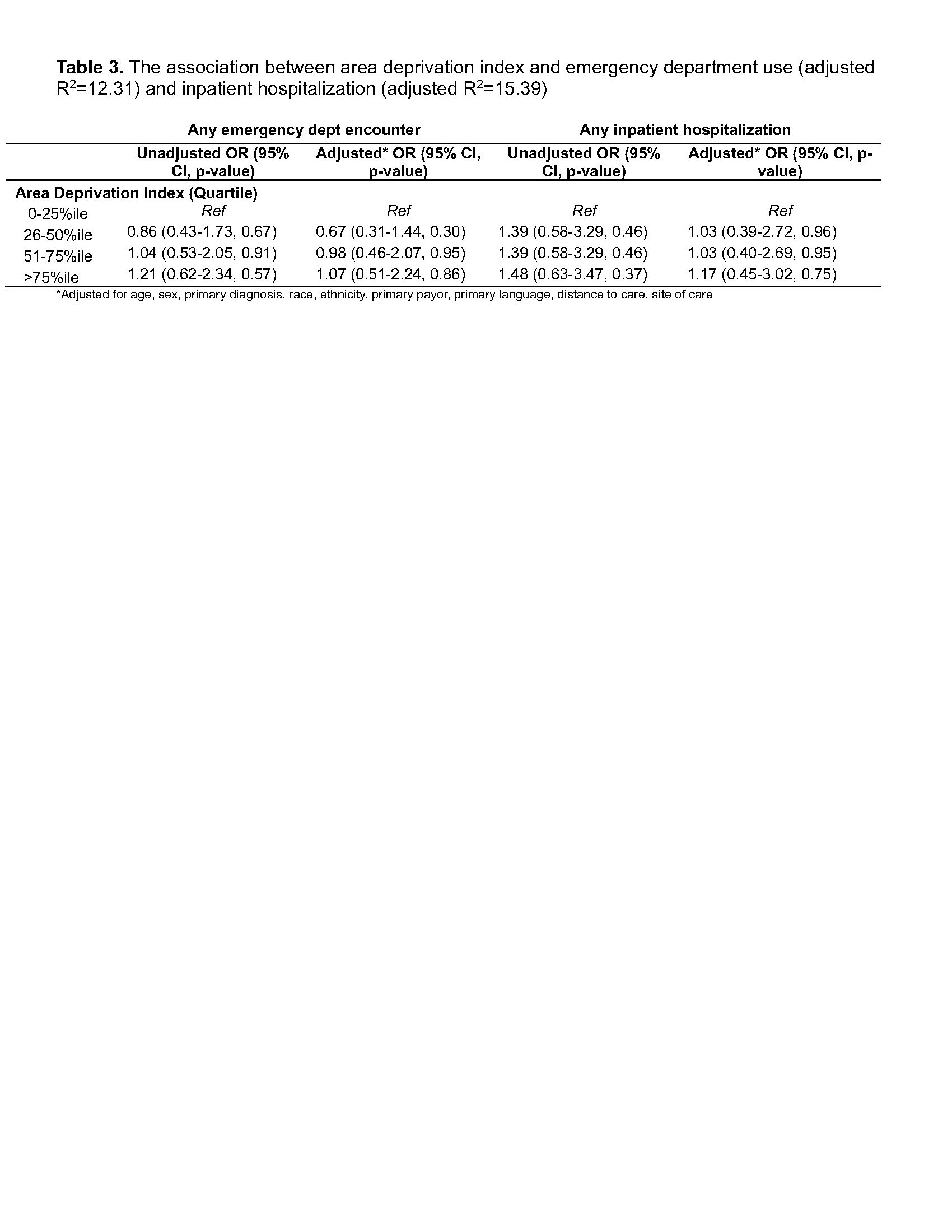
Results: Among 520 subjects with JIA (42%), SLE (17%), and other diseases, very low (20%) or low (24%) COI was associated with higher ED use, as compared to those with very high (9%) COI (Table 1). Inpatient hospitalization was lowest among those with very high (4%) COI. ADI and COI did not always correlate, as higher ADI scores (corresponding to higher neighborhood disadvantage) were seen in those with both very low (median 32, IQR 19-48) and high (median 34, IQR 11-54) COI. In adjusted analysis, low COI was associated with higher odds of emergency department use (adjusted odds ratio [aOR] 2.85, 95% CI 1.12-7.26) and inpatient hospitalization (aOR 4.15, 95% CI: 1.25-13.81 – Table 2), as compared to very high COI. Higher ADI scores were not associated with emergency department use or inpatient hospitalizations, in unadjusted or adjusted analysis (Table 3).
Conclusion: Neighborhood level social deprivation as measured by COI may be associated with worse outcomes among pediatric rheumatology patients, even accounting for other known causes of health disparities, such as minoritized race and lower socioeconomic status. Different social deprivation indices may not always yield similar results, as exhibited by the differences between COI versus ADI in our analysis. Similar analyses should be replicated in other geographic regions to understand if these results are generalizable. We suggest using multiple neighborhood level measures for studying health disparities in pediatric rheumatology patients, as they may measure distinct phenomena of local environment.
To cite this abstract in AMA style:
Soulsby W, Von Scheven E. Use of Geocoded Social Deprivation Indices to Understand Health Disparities in Pediatric Rheumatology [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/use-of-geocoded-social-deprivation-indices-to-understand-health-disparities-in-pediatric-rheumatology/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-geocoded-social-deprivation-indices-to-understand-health-disparities-in-pediatric-rheumatology/