Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Timely reproductive health conversations in the rheumatology outpatient setting are essential for optimal maternal-fetal health; however, the literature suggests that these conversations happen for only 50% of encounters with rheumatic disease patients of childbearing age. In this study, we gathered patient-reported insight into the difficulties encountered when discussing reproductive health issues in the outpatient setting in a primarily Hispanic population in urban Los Angeles.
Methods: A cross-sectional survey derived from the 2020 ACR Reproductive Health Guideline was distributed in English or Spanish to female patients ages 18-50 with systemic lupus erythematosus (SLE) or rheumatoid arthritis/juvenile idiopathic arthritis (inflammatory arthritis; IA) seen in our academic outpatient rheumatology clinic in the Los Angeles metropolitan area in late 2023. Participants were queried as to reasons they perceive difficulty in discussing contraception and pregnancy with their lupus/arthritis doctor; responses were analyzed based on participants’ diagnosis (SLE vs IA) and language preference (English vs Spanish). Questions regarding OB-GYN referral and language barriers were combined in all surveys and analyzed as a unit due to an unintentional error. Univariate logistic regression was used to assess the relationship between diagnosis, preferred language, and barriers to reproductive health discussions. A two-sided p-value of < 0.05 was considered statistically significant.
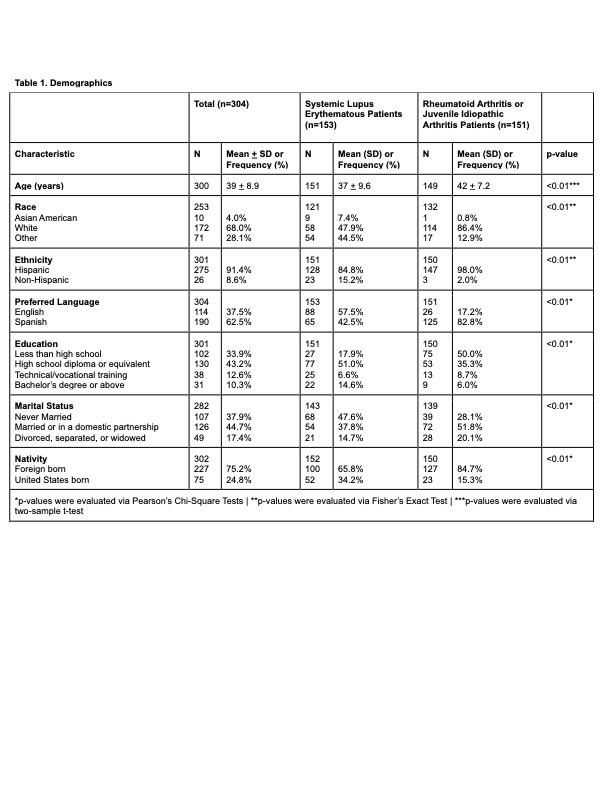
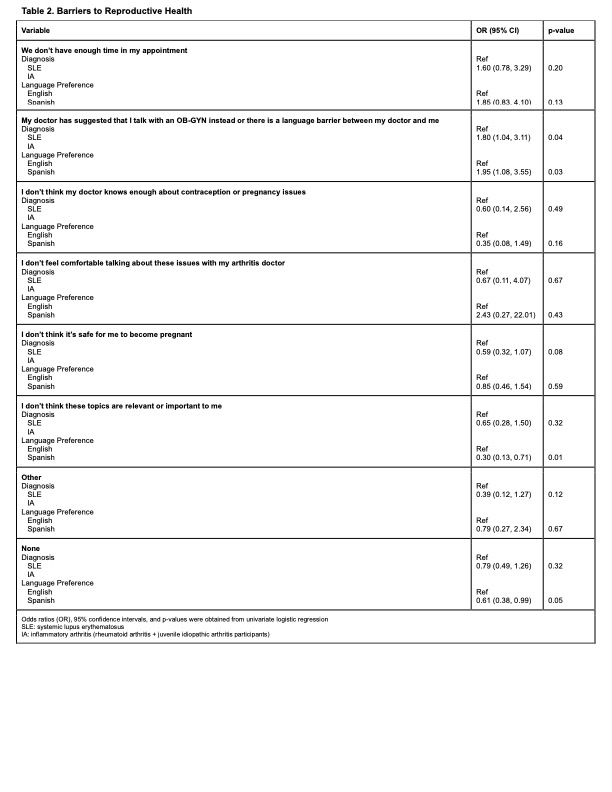
Results: 153 SLE and 151 IA participants were analyzed (Table 1). Most participants identified as Hispanic (91.4%) and had a Spanish survey preference (62.5%) (Table 1). Spanish respondents were more likely to note a deferral to OB-GYN or have a language barrier (OR 1.95; 95% CI 1.08-3.55; p=0.03), less likely to consider issues of reproductive health not relevant to them (OR 0.30; 95% CI 0.13-0.71; p=0.01) and less likely to report no barriers to reproductive health discussions (OR 0.61; 95% CI 0.38-0.99; p=0.05) vs. English respondents (Table 2). IA participants were more likely to be referred to an OB-GYN or have a language barrier (OR 1.80; 95% 1.04-3.11; p=0.04) and were borderline less likely to feel that pregnancy was unsafe for them (OR 0.59; 95% CI 0.32-1.07; p=0.08) compared with SLE patients (Table 2). There were no differences in appointment time, perceived clinician knowledge, or patient comfort level. Of note, 37.7% of SLE participants and 33.1% of IA participants noted no barriers to discussing reproductive health.
Conclusion: Our study sheds light on the patient’s perspective, and highlights language or OB-GYN referrals as limitations to engaging in reproductive health discussions with the rheumatologist. Further studies isolating language as a possible barrier are needed for non-English speaking populations. The large proportion of participants (over a third of the total) who had no barriers in discussing reproductive-related issues suggests that interventions targeting clinicians may also be helpful.
To cite this abstract in AMA style:
Delgado M, Hernandez-Tamayo C, Wilson M, Wise L. Patient-reported Difficulties Regarding Reproductive Health Discussions in an Urban Outpatient Setting [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patient-reported-difficulties-regarding-reproductive-health-discussions-in-an-urban-outpatient-setting/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-reported-difficulties-regarding-reproductive-health-discussions-in-an-urban-outpatient-setting/