Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) patients have higher cardiovascular (CV) risk compared to the general population, with a standardized CV mortality rate of 2-3 and 3-4 fold higher risk of venous thromboembolism (VTE). SLE-related risk factors contributing to these conditions have not been completely identified.
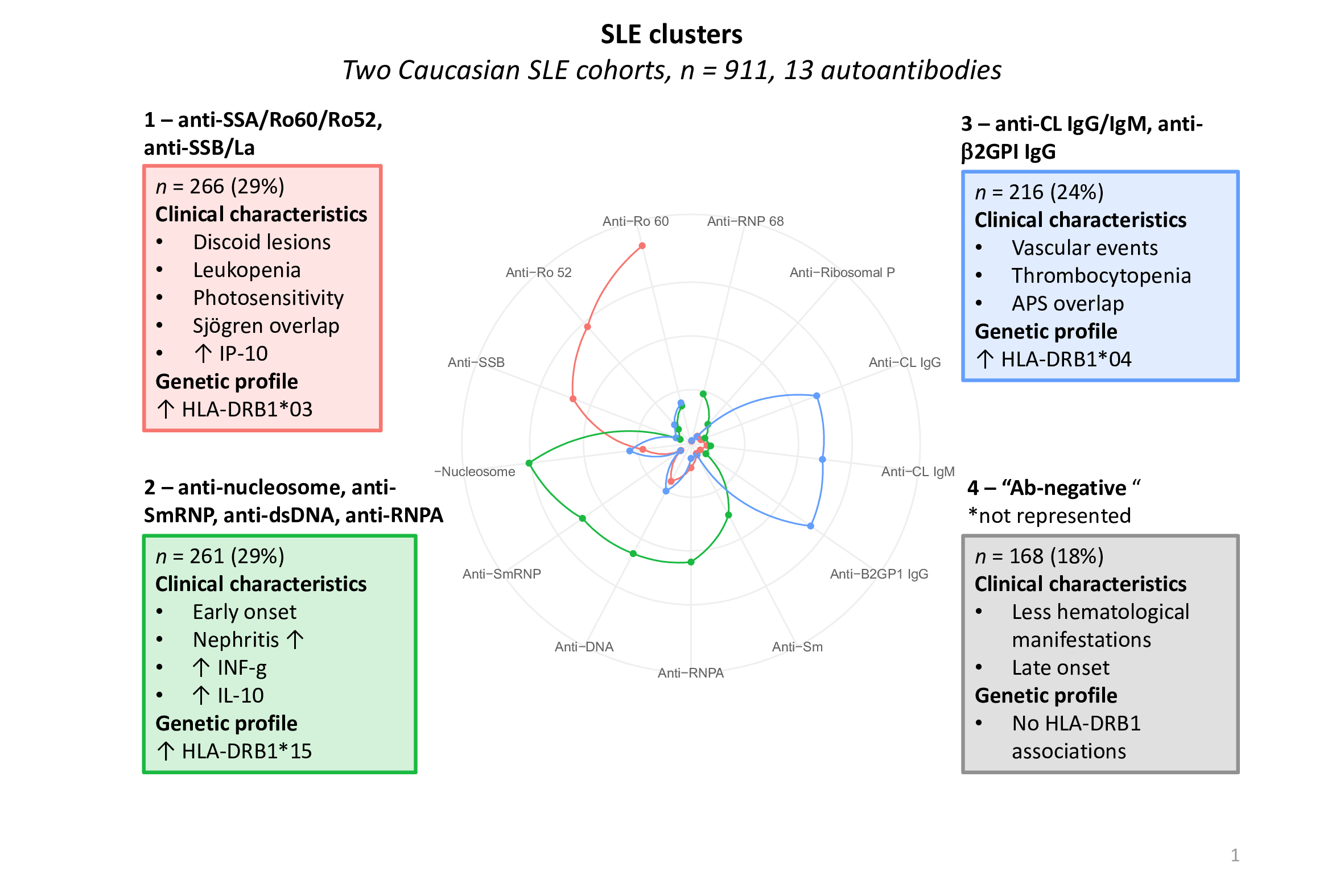
In a previous study, we identified four autoantibody-defined SLE clusters in 911 Caucasian SLE patients (1; Figure 1), associated with different HLA-DRB1 genotypes, clinical manifestations and cytokine patterns.
We compared the incidence rate of CV and VTE events in these clusters. The rate of events in each cluster was also compared to a general population control group.
Methods: In this prospective, cohort study, SLE patients aged 18-85, fulfilling ACR-1982 criteria, were included between 1995 and 2015. Four SLE clusters were defined based on cluster analysis of 13-autoantibodies. Each cluster was dominated by different autoantibodies, as described previously (1; Figure 1).
Individuals with history of CV events prior to the inclusion were excluded.
A control group without SLE was randomly selected from Total Population Register, matched on birth, sex, residence 10:1 to each SLE patient.
“Hard” vascular outcomes were defined using ICD codes from National Patient Register (NPR): ischemic heart disease (IHD), cerebrovascular disease, peripheral arterial disease, heart failure, VTE. Data on death due to CV events were extracted from the Cause of Death Register.
End of follow-up was death, migration, end of study (December 2022) or first event.
History of hypertension, diabetes and chronic kidney disease were assessed using ICD-coded visits from the NPR before inclusion in patients and controls. Smoking habit, BMI, cholesterol levels, C3, C4, disease duration, SLE clinical manifestations, SLEDAI-2K score, SLICC Damage Index were collected at inclusion in SLE.
Incidence rates (IR) for outcomes were calculated. Hazard ratios and 95% confidence intervals (HR; 95% CI) from age-adjusted Cox proportional hazards models were used to estimate the relative risk of incident vascular events comparing clusters using cluster 4 as a reference and comparing each cluster to a general population control group.
Results: 460 SLE patients and 4271 controls were included with a mean follow-up of 14.2 years (SD 5.8).
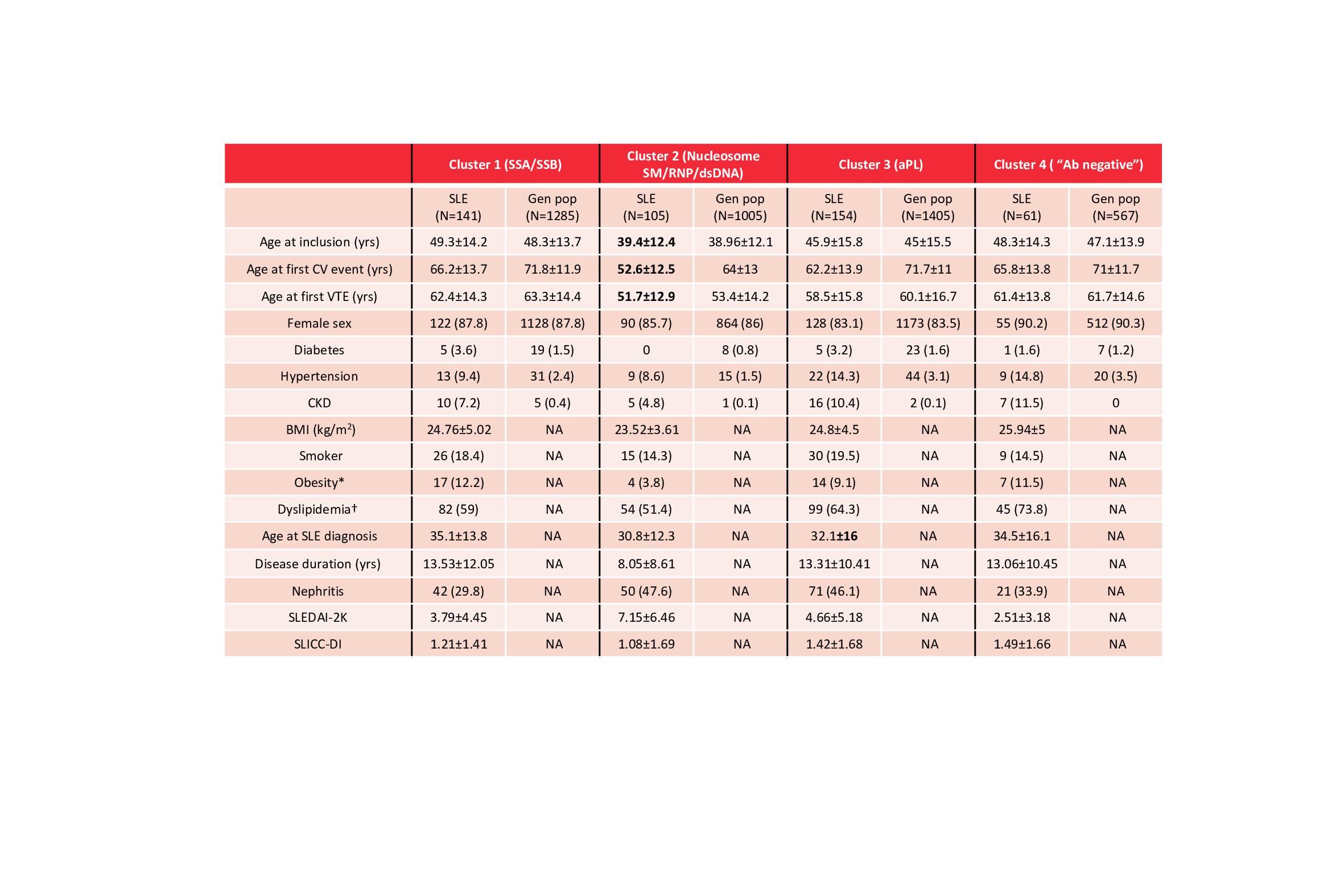
Table 1 shows the characteristics of our population. SLE were younger at first event compared to controls. SLE patients in cluster 2 were younger at inclusion and younger at first CV/VTE event compared to the others.
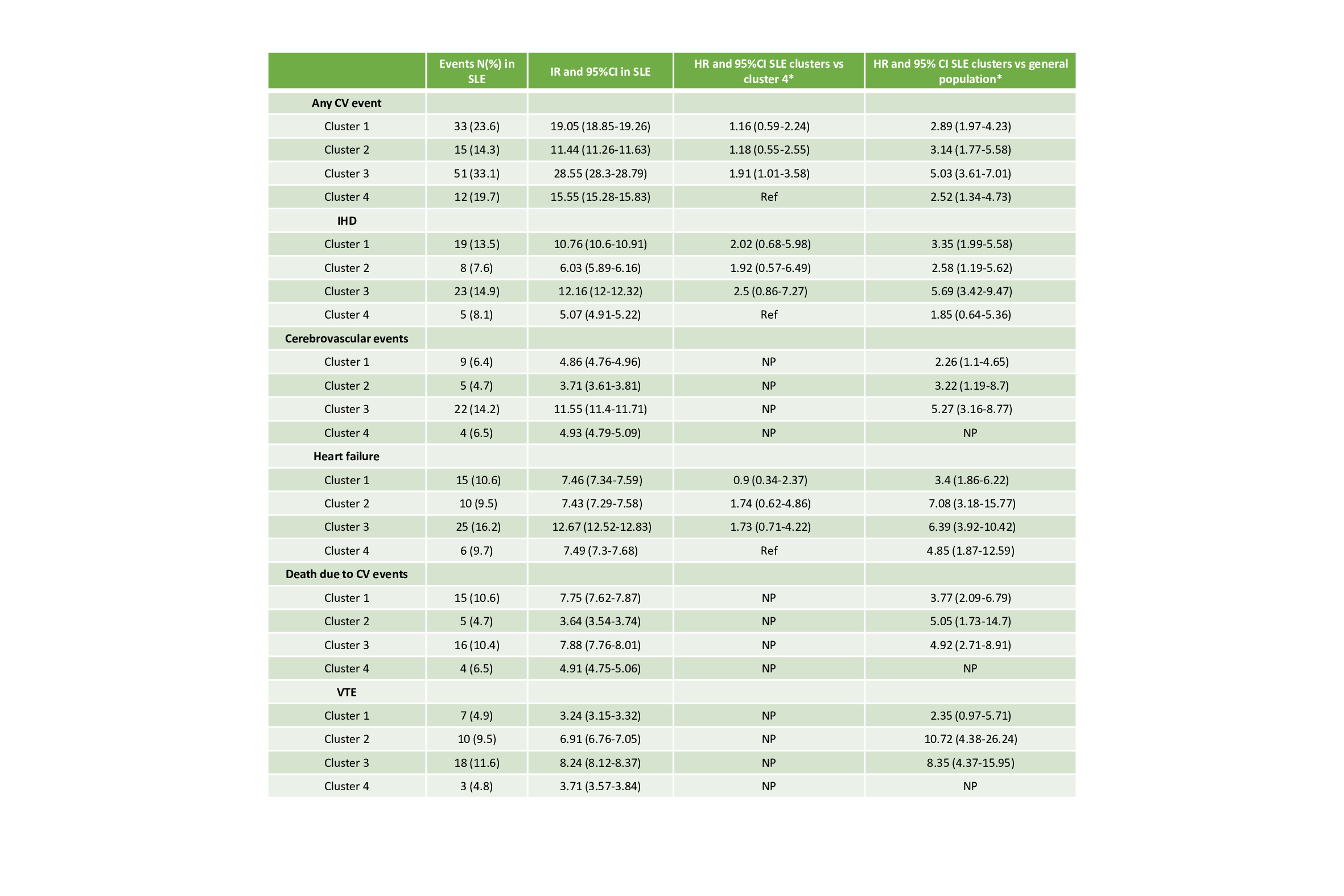
Cluster 3 had the highest crude IR for CV outcomes and VTE compared to the others. The risk of any CV event in cluster 3 was almost two times the risk of cluster 4 (age-adjusted HR 1.91, 95%CI 1.01-3.58; Table 2). Cluster 2 and cluster 3 had almost two-times higher risk of heart failure compared to the others (Table 2). Notably, HR for IHD did not differ between cluster 4 and controls (Table 2).
Conclusion: Risk of vascular events in SLE is driven by specific disease subsets, characterized by autoantibody profiles. A higher risk was observed in the “aPL positive” cluster 3, and a lower risk in the “autoantibody-negative” cluster 4.
References
1. Diaz-Gallo LM et al. ACR Open Rheum. 2022.
Patients underwent an unsupervised cluster analysis based only on 13 autoantibodies
An autoantibody was considered dominant in a subgroup if it was present in at least 50% of patients in that cluster
Continuous variables are expressed as mean ± standard deviation (SD) and categorical variables are expressed as number (percentage) of participants.
CV: cardiovascular; VTE: venous thromboembolism; CKD: chronic kidney disease; BMI: body mass index; APS: antiphospholipid antibody syndrome; SLICC-DI: SLICC-damage index PDN:prednisone; NA:not available.
*Obesity was defined as: BMI≥30 kg/cm2.
† Dyslipidemia was defined as: total cholesterol>6.2 mmol/L and/or LDL> 4.1 mmol/L and/or HDL <1.03 mmol/L and/or triglycerides >1.7 mmol/L and/or ongoing cholesterol-lowering treatment.
N= total number of events in each cluster. %=(N of events/N total in each cluster)*100. CV: cardiovascular; IHD: ischemic heart disease; VTE: venous thromboembolism; NP=not performed. *Age-adjusted models. Incidence rates are calculated for 1000 person-years and CI are calculated using the Poisson distribution.
Any CV event= IHD+stroke+other cerebrovascular events+peripheral arterial thrombosis or embolism+heart failure+death due to CV events; Cerebrovascular events=stroke+other cerebrovascular events+cerebral hemorrhages; VTE=deep venous thrombosis+pulmonary embolism.
To cite this abstract in AMA style:
Ferrigno S, Arkema E, Diaz-Gallo L, Gunnarsson I, Zickert A, Svenungsson E. Incidence of Cardiovascular and Venous Thromboembolic Events in Four Autoantibody-defined Systemic Lupus Erythematosus Clusters [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/incidence-of-cardiovascular-and-venous-thromboembolic-events-in-four-autoantibody-defined-systemic-lupus-erythematosus-clusters/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-of-cardiovascular-and-venous-thromboembolic-events-in-four-autoantibody-defined-systemic-lupus-erythematosus-clusters/