Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) patients have an increased cardiovascular (CV) risk compared to the general population. Although SCORE2 (systematic coronary risk evaluation 2) has improved the CV risk determination of the SCORE, it is still far from being well established in SLE. For this purpose, the research of tools that may identify high-risk SLE patients who may benefit from active therapy to prevent CV events is of major importance. The main objective is to determine if the use of carotid ultrasound may improve the stratification of CV risk determined by the SCORE2 in SLE patients.
Methods: Cross-sectional study of 161 SLE patients in which CV risk was initially categorized according to the SCORE2. Secondly, all of them underwent a carotid ultrasound for measurement of carotid intima-media thickness (C-IMT) and detection of carotid plaques. The presence of carotid plaque directly includes patients in the very high cardiovascular risk category.
Results: We included a total of 161 SLE patients of whom 27 were excluded from the final analysis because of very high CV risk (17 due to previous CV event, 6 Diabetes Mellitus (DM) and 4 chronic kidney disease (CKD).
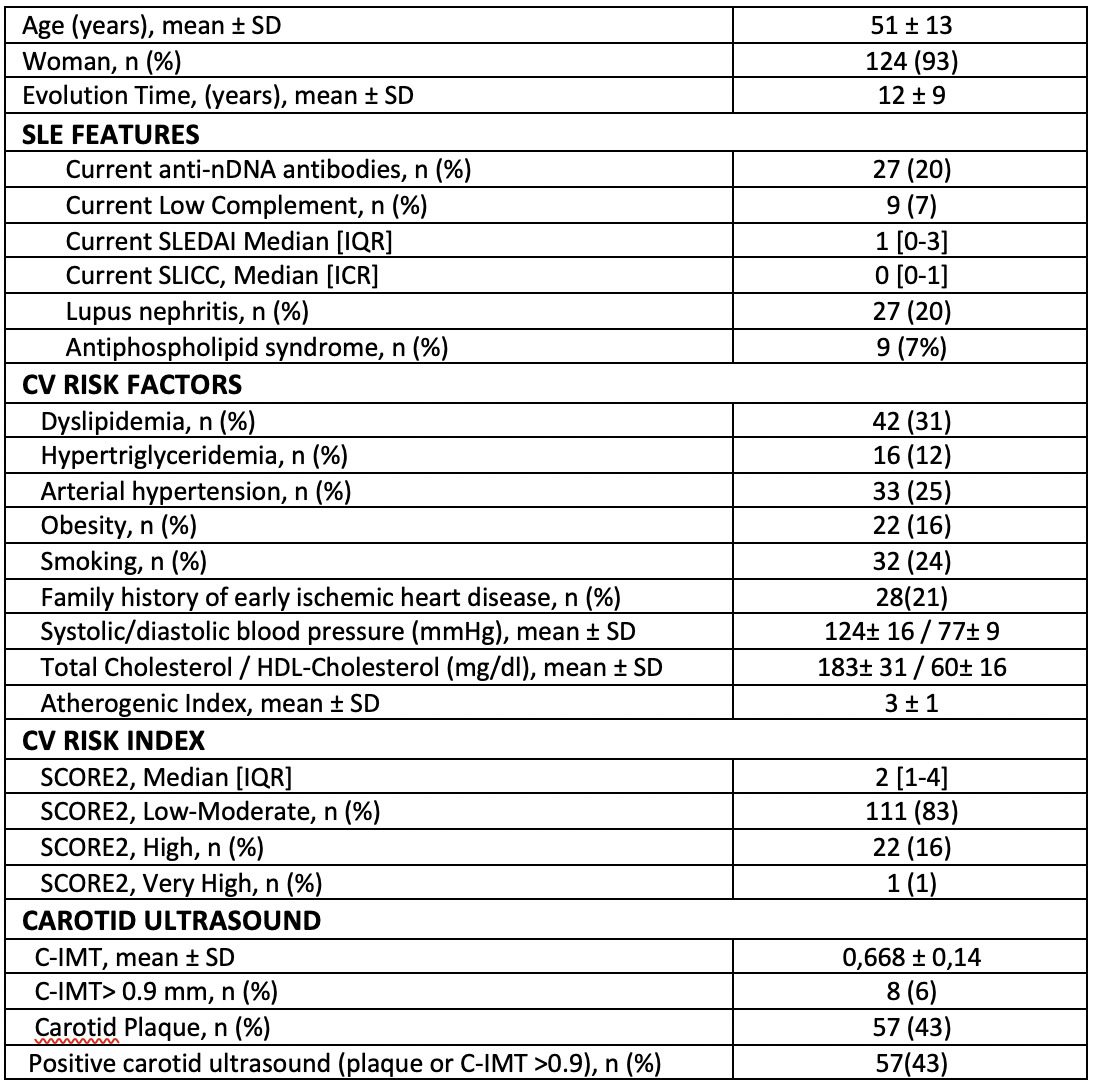
The main characteristics of the remaining 134 patients included are shown in Table 1. Ninety-three percent of the patients were women with a mean age of 51 ± 13 years and disease duration of 12 ± 9 years. From the 134 patients, 43% (57) had carotid plaques.
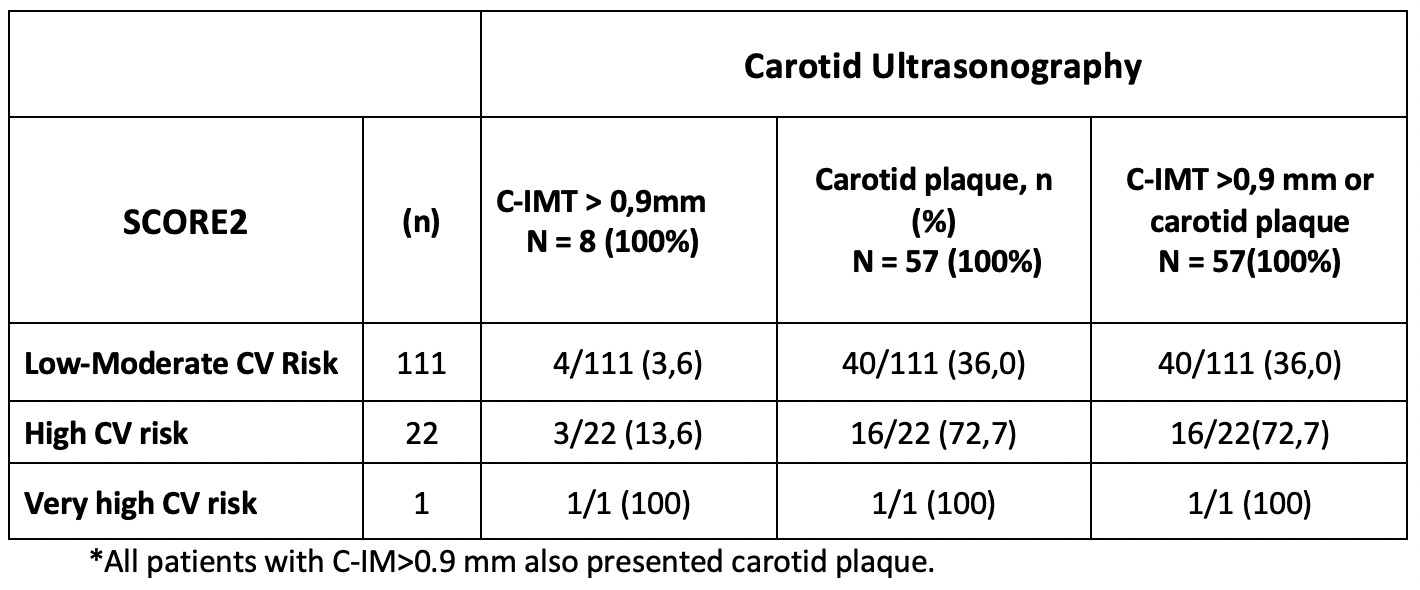
Using SCORE2, patients were classified into 3 CV risk groups, low-moderate risk (111 cases, 83%), high risk (22, 16%) and very high risk (1, 1%). Table 2 shows the results of the carotid ultrasound study in relation to the CV risk groups classified by SCORE2. According to C-IMT, only 3.6% (4/111) of patients with low-moderate risk with SCORE2 and 13.6% (3/22) of patients with high risk were reclassified as very high CV risk (C-IMT > 0.9 mm). However, carotid plaque detection reclassified 36% (40/111) of patients with low-moderate risk by SCORE2 and 72.7% (16/22) of patients with high CV risk as very high CV risk.
In addition, all patients with C-IMT > 0.9 mm were found to have carotid plaque.
Conclusion: The presence of carotid plaque reclassifies to very high CV risk a significant number of SLE patients with low-moderate CV risk by SCORE2. The C-IMT study does not add any value to the carotid plaque study in the stratification of CV risk.
Disclosures: C. Corrales Selaya: None; C. Bejerano: None; C. Secada Gómez: None; V. Portilla-González: None; R. Blanco-Alonso: AbbVie, 2, 5, 6, Bristol-Myers Squibb, 2, 6, Galapagos, 6, Janssen, 2, 6, Lilly, 2, 6, MSD, 2, 5, 6, Pfizer, 2, 6, Roche, 2, 5, 6; V. Martinez Taboada: None; L. Riancho: None; a. Corrales-Martínez: None.
To cite this abstract in AMA style:
Corrales Selaya C, Bejerano C, Secada Gómez C, Portilla-González V, Blanco-Alonso R, Martinez Taboada V, Riancho L, Corrales-Martínez a. Cardiovascular Risk in Systemic Lupus Erythematosus: Carotid Ultrasonography Is Useful for the Re-stratification of Cardiovascular Risk Determined by Score2 [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-risk-in-systemic-lupus-erythematosus-carotid-ultrasonography-is-useful-for-the-re-stratification-of-cardiovascular-risk-determined-by-score2/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-risk-in-systemic-lupus-erythematosus-carotid-ultrasonography-is-useful-for-the-re-stratification-of-cardiovascular-risk-determined-by-score2/