Session Information
Date: Sunday, November 17, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Individuals with axial spondyloarthritis (axSpA) have a risk of fracture that is nearly double that of the general population, possibly related to chronic inflammation. Vertebral fracture risk may be due to regional osteopenia paired with regions of excess bone stiffness. We assessed the impact of treatment with tumor necrosis factor inhibitors (TNFi) and non-biologic disease-modifying antirheumatic drugs (DMARDs) on hip and spine fractures in axSpA, relative to nonsteroidal anti-inflammatory drugs (NSAIDs).
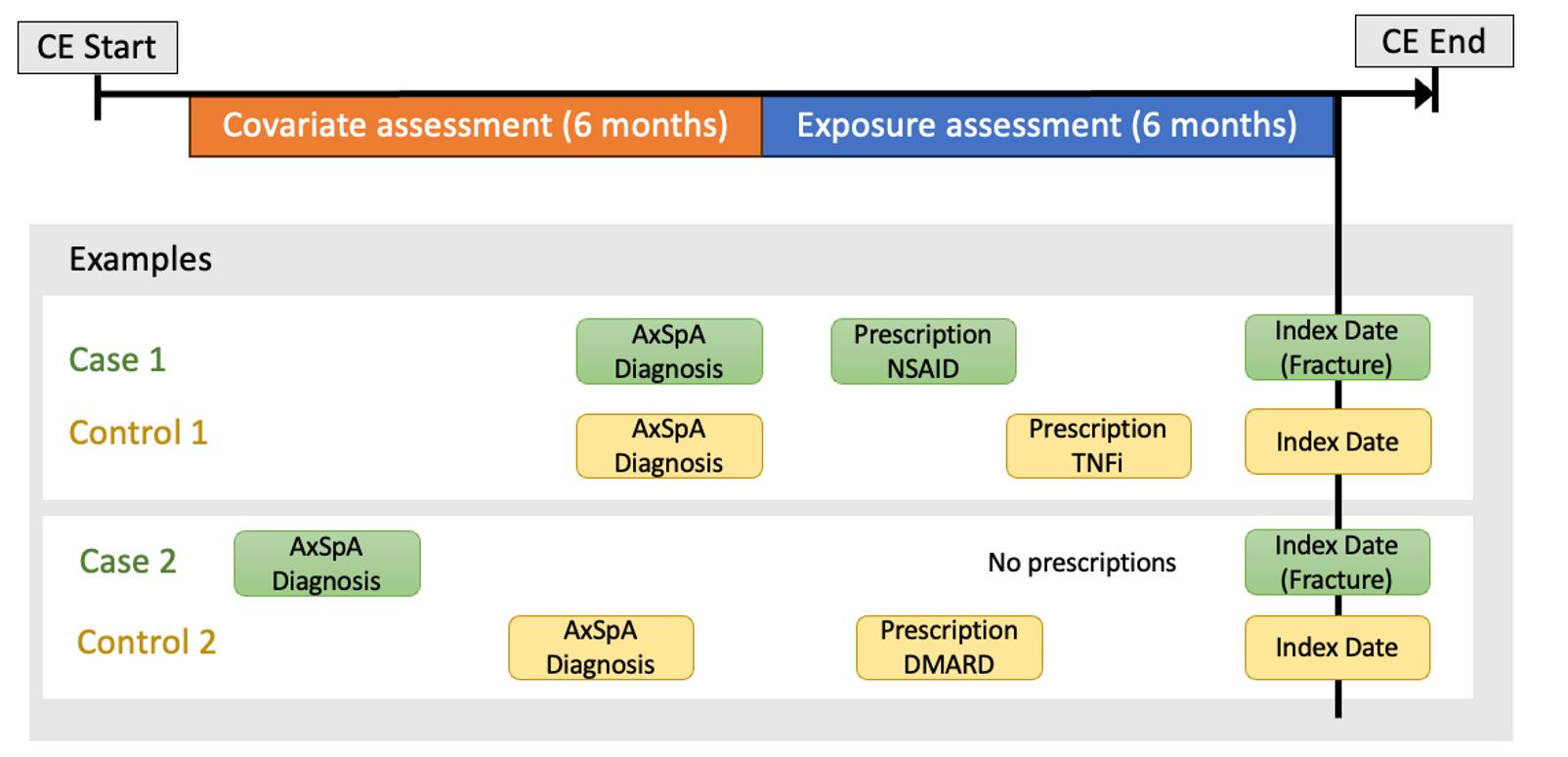
Methods: We conducted a nested case-control study using 2006-2021 data from the US-based MerativeTM MarketScan® Database (Figure 1). We included adults 18-65 years old with ≥1 inpatient or ≥2 outpatient axSpA ICD-9 or 10 diagnosis codes. The primary outcome was hip and/or spine fracture, defined by diagnosis or procedure codes. For each fracture case, we selected up to 10 controls without fracture. We evaluated medication use hierarchically (TNFi, DMARDs, NSAIDs [referent], or none) using pharmacy claims and procedure codes (for infusions). We assessed the odds of hip or spine fracture with medication class using unconditional logistic regression with adjustment for potential confounders.
Results: Our main analysis included 13,519 individuals with axSpA, comprising 1,229 hip/spine fracture cases and 12,290 controls. Hip/spine fracture occurred in 9% of the study sample. Among fracture cases, 25% were TNFi users, 9% were DMARD users, 18% were NSAID users and 48% were not on any medication. Individuals on TNFi had 29% lower odds of fracture compared to those on NSAIDs (OR 0.71, 95% CI 0.59-0.85), accounting for age, sex, and diagnosis year (Figure 2). Results for TNFi were similar in the fully adjusted model (OR 0.75, 95% CI 0.62-0.91) and when stratified by sex. There was no protective effect of DMARDs.
Conclusion: Using a large US insurance claims database, we observed a protective effect of TNFi on hip/spine fractures in axSpA compared with use of NSAIDs or DMARDs. These findings suggest a beneficial effect of TNFi in bone remodeling in axSpA. By reducing systemic inflammation and slowing local bone remodeling, TNFi use may help preserve both bone density and architecture, thus lowering risk for fractures. Further research investigating the impact of timing of TNFi initiation and alternative axSpA treatment modalities, such as IL-17 inhibitors and Janus kinase (JAK) inhibitors, on fractures will enhance understanding of how to mitigate fracture risk in axSpA.
To cite this abstract in AMA style:
Driscoll D, George N, Jafarzadeh S, Peloquin C, Liew J, Dubreuil M. Risk of Hip and Spine Fractures in Axial Spondyloarthritis Is Associated with Treatment Class [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/risk-of-hip-and-spine-fractures-in-axial-spondyloarthritis-is-associated-with-treatment-class/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-hip-and-spine-fractures-in-axial-spondyloarthritis-is-associated-with-treatment-class/