Session Information
Date: Sunday, November 17, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Definitions for active and structural lesions on MRI of the SI joints (MRI-SIJ) typical of axial SpA (axSpA), proposed by de Hooge and the ASAS MRI study group, were assessed for their predictive validity.(de Bruin et al. 2024) However, the MRI study group active lesions definition has not been compared with the current ASAS definition for positive MRI-SIJ (ASAS-MRI-SIJ+), nor combinations of active lesions and structural lesions have been assessed. We aimed to compare the proposed MRI study group definition for active lesions with that of ASAS-MRI-SIJ+ and evaluate the predictive validity of different combinations of active lesions and structural lesions.
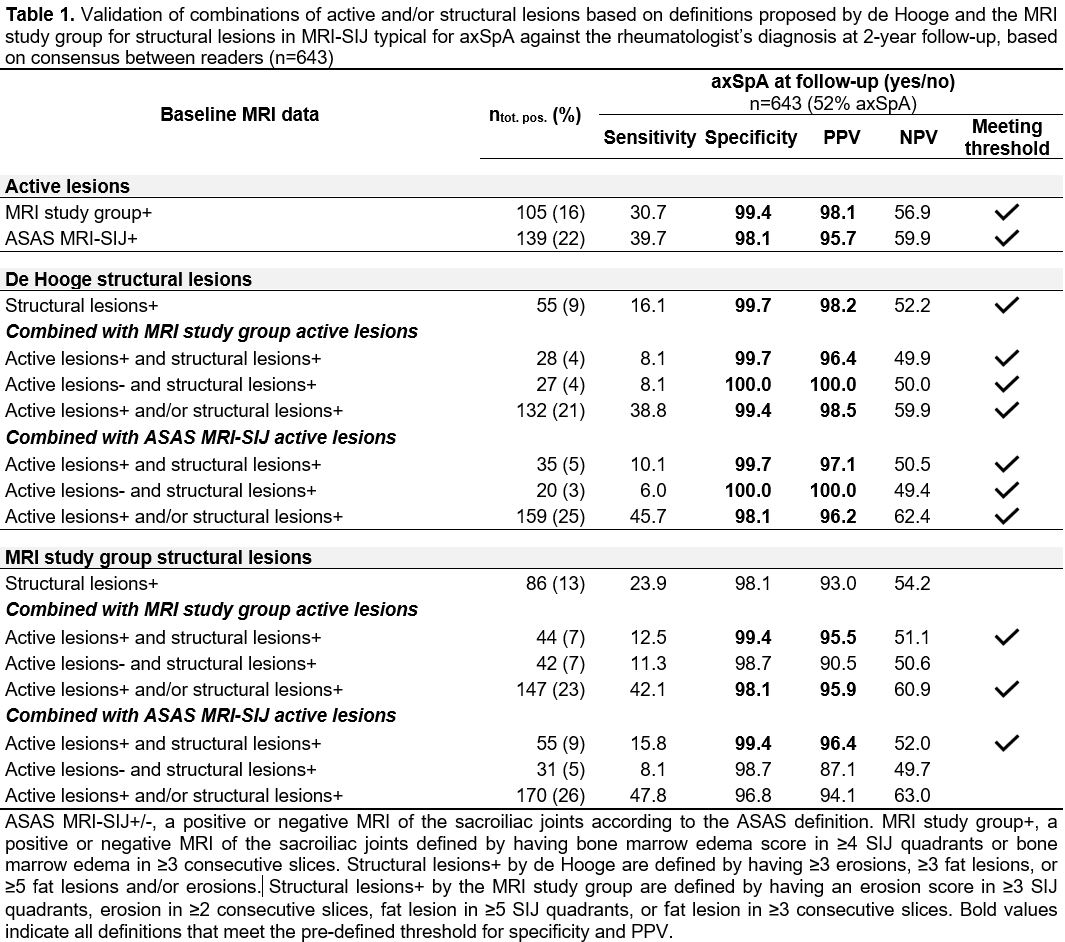
Methods: Patients with chronic back pain (≥3 months; ≤2 years; onset < 45 years) from the SPondyloArthritis Caught Early (SPACE) inception cohort had a two-year follow-up at which they were diagnosed by a rheumatologist as axSpA or no-axSpA. Patients with a ‘definite’ (level of confidence about the diagnosis ≥7) or ‘most likely’ (level of confidence < 7 and a consistent diagnosis in the last 2 visits) diagnosis were included in this analysis. Three central readers assessed baseline MRI-SIJ for bone marrow edema, erosions, and fat lesions. MRI-SIJ data that were available for ≥2 readers were analyzed for the consensus between ≥2 readers on scored lesions. Different combinations of active lesions and/or structural lesions were created based on the component definitions of de Hooge, MRI study group and ASAS-MRI-SIJ+ (Table 1). Sensitivity, specificity, positive and negative predictive values (PPV and NPV) were calculated for each combination. Definitions with a specificity ≥95% and PPV ≥95% were accepted.
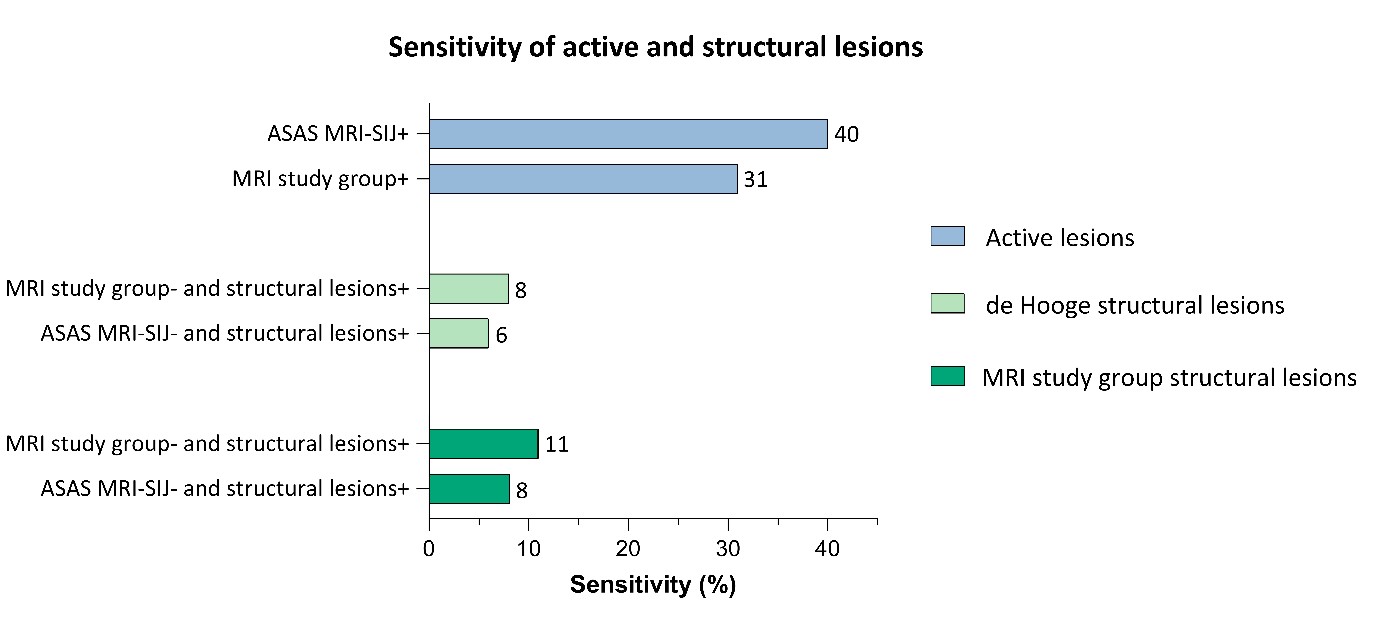
Results: In total, we analyzed 643 patients (age 30 (SD 8) years; 39% males; 52% axSpA). Active lesions as defined by the ASAS-MRI-SIJ+ performed best by having higher sensitivity (40% vs 31%) with similar specificity compared to the active lesions of the MRI study group (98% vs 99%) (Table 1). All combinations of active lesions and structural lesions by de Hooge met the threshold, while the structural lesions of the MRI study group met the threshold only in presence of active lesions. Structural lesions alone (i.e. without active lesions) contributed with only a small gain in sensitivity, between 6-11% (Figure 1).
Conclusion: The current ASAS-MRI-SIJ+ definition performs better than the new MRI study group active lesions proposal. Structural lesions have only a small gain in sensitivity for identifying axSpA in this group of patients with short symptom duration. In combining active lesions and structural lesions, ASAS-MRI-SIJ+ and de Hooge structural lesions have the best performance.
To cite this abstract in AMA style:
de Bruin L, Marques M, van Lunteren M, de hOoge M, Exarchou S, Minde Fagerli K, Ramonda R, Landewé R, van Gaalen F, van der Heijde D, Ramiro S. Performance of Combined MRI SI Joint Active and Structural Lesions in Diagnosing Axial SpA: A Prospective Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/performance-of-combined-mri-si-joint-active-and-structural-lesions-in-diagnosing-axial-spa-a-prospective-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-combined-mri-si-joint-active-and-structural-lesions-in-diagnosing-axial-spa-a-prospective-cohort-study/