Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: ANCA-associated vasculitis (AAV) is a frequently relapsing disease for which a meta-analysis concluded that an increase or persistence of ANCA during remission is only moderately predictive of future disease relapse and that serial ANCA measurements during remission are of limited use in guiding treatment decisions for individual patients. However, this analysis analyzed heterogeneous ANCA assays and combined different subgroups of AAV patients or PR3 and MPO-AAV patients, whereas granulomatosis with polyangiitis (GPA) and PR3-AAV have a higher relapse risk. We investigated whether serial ANCA testing with a uniform ELISA assay could be of interest in predicting relapse risk in a cohort of GPA patients.
Methods: To be included, patients had to have GPA follow-up at our National Referral Center, at least two measurements of ANCA titer by ELISA less than 12 months apart during inactive disease, and an assessment of disease activity within 18 months of the second ANCA titer measurement. The primary objective was to evaluate the association of an increase in ANCA titer at the time of inactive disease with any relapse. The primary endpoint was the cumulative incidence of relapse within the following 18 months. To obtain confounder-adjusted relapse-free survival curves for each group, we used direct standardization (G-computation) using a Cox regression model. The results were analyzed globally in time periods where patients had an increased ANCA titer (Increase group) compared to those without (No increase group) and in a subgroup of PR3-AAV patients. We also estimated 18-month adjusted restricted mean survival times (RMST). In a sensitivity analysis, we compared patients with ANCA doubling versus no doubling.
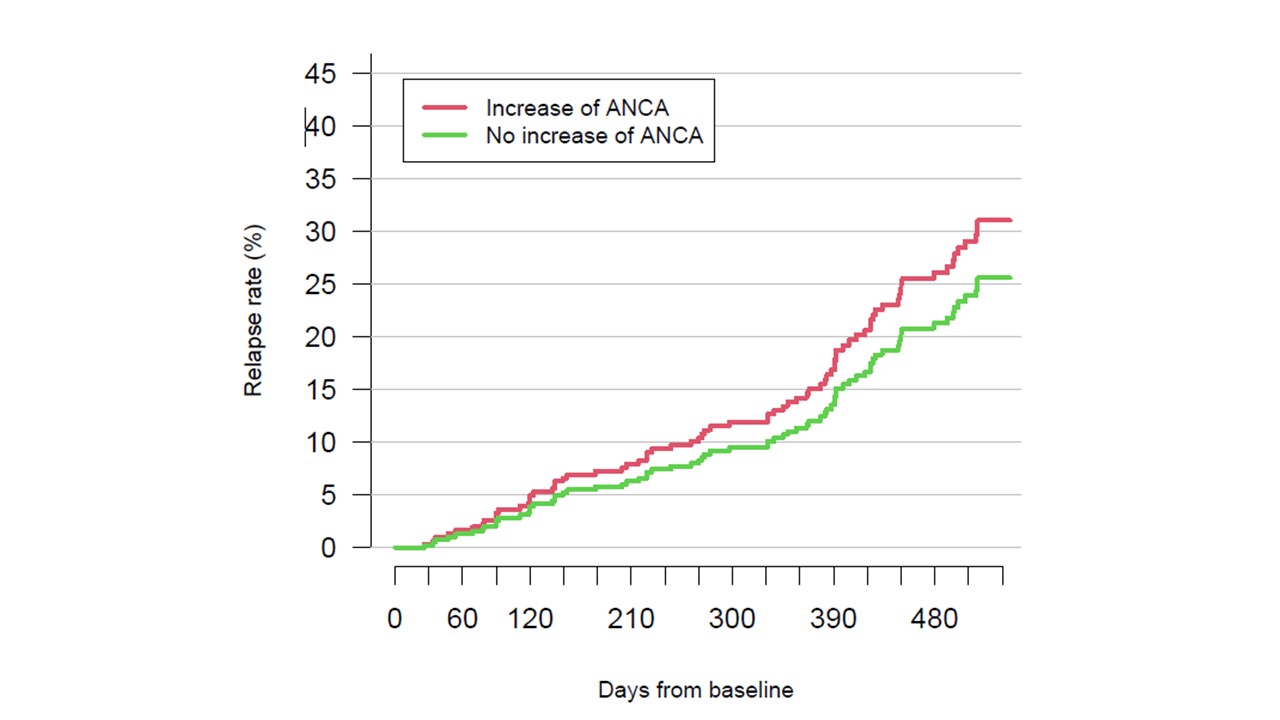
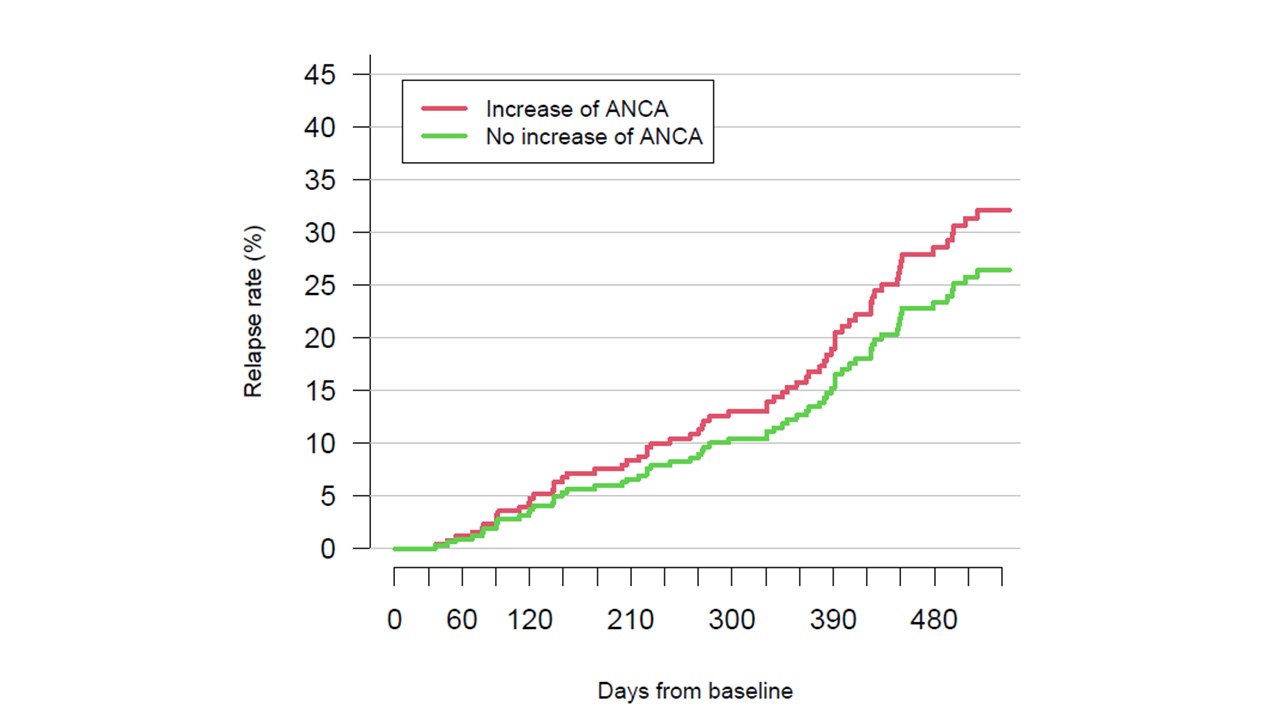
Results: 125 GPA patients were analyzed in the primary analysis (PR3-ANCA: 105; MPO-ANCA: 20) for a total of 378 patient-periods. We observed 74 relapses, 7 out of 23 patient-periods in the Increase group (unadjusted relapse rate: 33.8%) vs. 67 out of 355 patient-periods in the No increase group (unadjusted relapse rate: 25.5%). Of the 23 periods of increased ANCA levels, 16 were not followed by a relapse. The adjusted relapse rates were 31.0% (11.2−54.4) vs. 25.6% (19.7−31.9), respectively (Fig. 1). The adjusted risk of major relapse was 24.9% (7.0−45.5) vs. 16.5% (12.3−21.9). In 105 PR3-ANCA patients, the corresponding relapse rate was 32.1% (11.9−54.1) vs. 26.4% (20.4−34.0) (Fig. 2). When restricted to patients with a doubling of the ANCA titer, the relapse rate was 36.2% (15.1−61.4) in 20 patient-periods vs. 25.3% (19.6−31.6) in 358 patient-periods. The difference in RMST between patients with and without an increased ANCA titer was -13.3 (-75.7−33.3) days, -14.2 (-80.8−33.9) days and -27.1 (-100.7−22.2) days for all patients, PR3-ANCA patients and patients with a doubling of the ANCA titer, respectively.
Conclusion: Despite using the same ELISA test consistently over time in a homogeneous population of GPA patients followed at a reference center, the predictive value of an increase in ANCA, a doubling of ANCA or an increase in PR3-ANCA alone is not sufficient to predict relapse at 18 months to consider escalating treatment on an individual basis.
To cite this abstract in AMA style:
Puéchal X, Iudici M, Perrodeau E, Goulvestre C, cohen P, Régent A, Mouthon L, Guillevin L, Porcher R, Terrier B. Does Serial ANCA Testing Help Predict the Risk of Relapse in Granulomatosis with Polyangiitis? A Single-center Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/does-serial-anca-testing-help-predict-the-risk-of-relapse-in-granulomatosis-with-polyangiitis-a-single-center-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-serial-anca-testing-help-predict-the-risk-of-relapse-in-granulomatosis-with-polyangiitis-a-single-center-cohort-study/