Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: SLE is a chronic autoinflammatory condition affecting multiple organ systems. Patients with SLE are at a higher risk for infection compared to the general population, both due to the autoinflammatory nature of the disease and its immunosuppressive therapy. Influenza has also been associated with SLE flares requiring hospitalization. This study aimed to assess the trends, outcomes, and predictors of mortality in SLE patients who were hospitalized for influenza.
Methods: The National Inpatient Sample (NIS) databases (2015–2020) of the Healthcare Cost and Utilization Project (HCUP) were used. We applied discharge weight (DISCWT) provided in the database to generate the national estimates. Pearson Chi-square test for categorical variables and Student’s t-tests/one-way ANOVA for continuous variables were applied to compare the baseline demographics and hospital characteristics between the groups. Matched propensity score analysis was used to account for confounding.
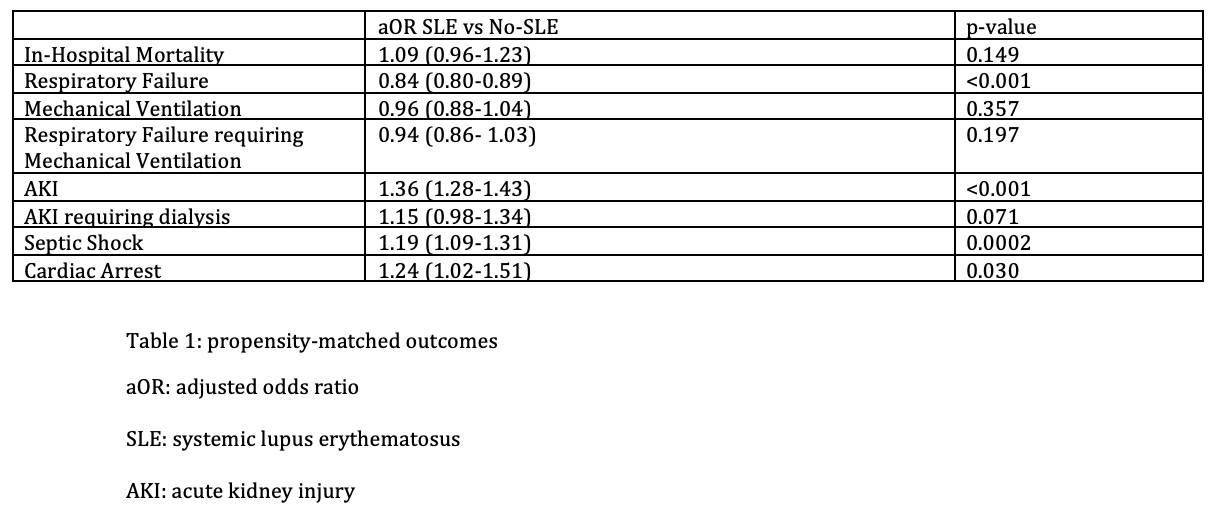
Results: A total of 9370 patients with SLE and 1,306,110 patients without SLE admitted for influenza infection were studied. The mean age was 55 and 66 years respectively. The group with SLE was more female predominant at 88%. Propensity-matched outcomes between the two groups showed no statistical difference in in-hospital mortality, however, there were higher odds of respiratory failure (aOR: 0.84; CI 0.80-0.89; p-value < 0.001), acute kidney injury (AKI) (aOR: 1.36; CI 1.28-1.43; p-value < 0.001), and cardiac arrest (aOR 1.24; CI 1.02-1.51; p-value 0.03) in the SLE group (table 1). The significant predictors of mortality among SLE patients were age, chronic lung disease, presence of coronary artery disease including prior myocardial infarction and coronary artery bypass graft, and obesity. The number of patients hospitalized for influenza with SLE increased from the year 2015 to 2018 and decreased afterward from 2019 to 2020. SLE patients had significantly higher hospitalization costs compared to non-SLE patients (median cost $8399.28 vs $7646.49 respectively, p-value < 0.001)
Conclusion: SLE does not affect the in-hospitality mortality rates in those admitted with influenza, however, it does lead to worse outcomes in the form of respiratory failure, AKI, and cardiac arrest. SLE patients also incur higher costs compared to non-SLE patients. Further efforts should be made to ensure SLE patients are vaccinated against influenza to avoid worse hospital outcomes.
To cite this abstract in AMA style:
Khanfar A, Cooper S, Mohamed A, Borse T, Nalwalla S. Trends, Outcomes, and Predictors of Mortality in Patients with SLE Hospitalized for Influenza [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/trends-outcomes-and-predictors-of-mortality-in-patients-with-sle-hospitalized-for-influenza/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-outcomes-and-predictors-of-mortality-in-patients-with-sle-hospitalized-for-influenza/