Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Chronic nonbacterial osteomyelitis (CNO) is a rare autoinflammatory bone disorder. Some patients with CNO may present acutely and be misdiagnosed as infectious osteomyelitis (IO). Understanding the initial presentation and disease course may help to improve clinical care through early identification and appropriate treatment. The purpose of this study is to review a cohort of patients with a clinical diagnosis of culture-negative IO and describe the similarities and differences of those who subsequently develop CNO.
Methods: A retrospective chart review was conducted at a single U.S. tertiary care pediatric hospital. Inclusion criteria were: (1) diagnosed with IO between January 2014 and December 2023, (2) age between 0.5 and 18 years at presentation, (3) blood and/or bone cultures negative, positive for a likely contaminant, or not obtained. The exclusion criteria were: (1) preceding injury, surgery, or hardware placement, (2) immunosuppressed, (3) involvement of only phalanges. Demographic, clinical, laboratory, imaging, and therapeutic data from eligible patients was collected. Descriptive data was extracted from visit notes to determine if there was complete, partial, or no response to antibiotics. If patients were later diagnosed with CNO by a pediatric rheumatologist they were classified in the CNO cohort, and Persistent IO if not. Nonparametric statistics were performed to compare the characteristics between the CNO and Persistent IO cohorts.
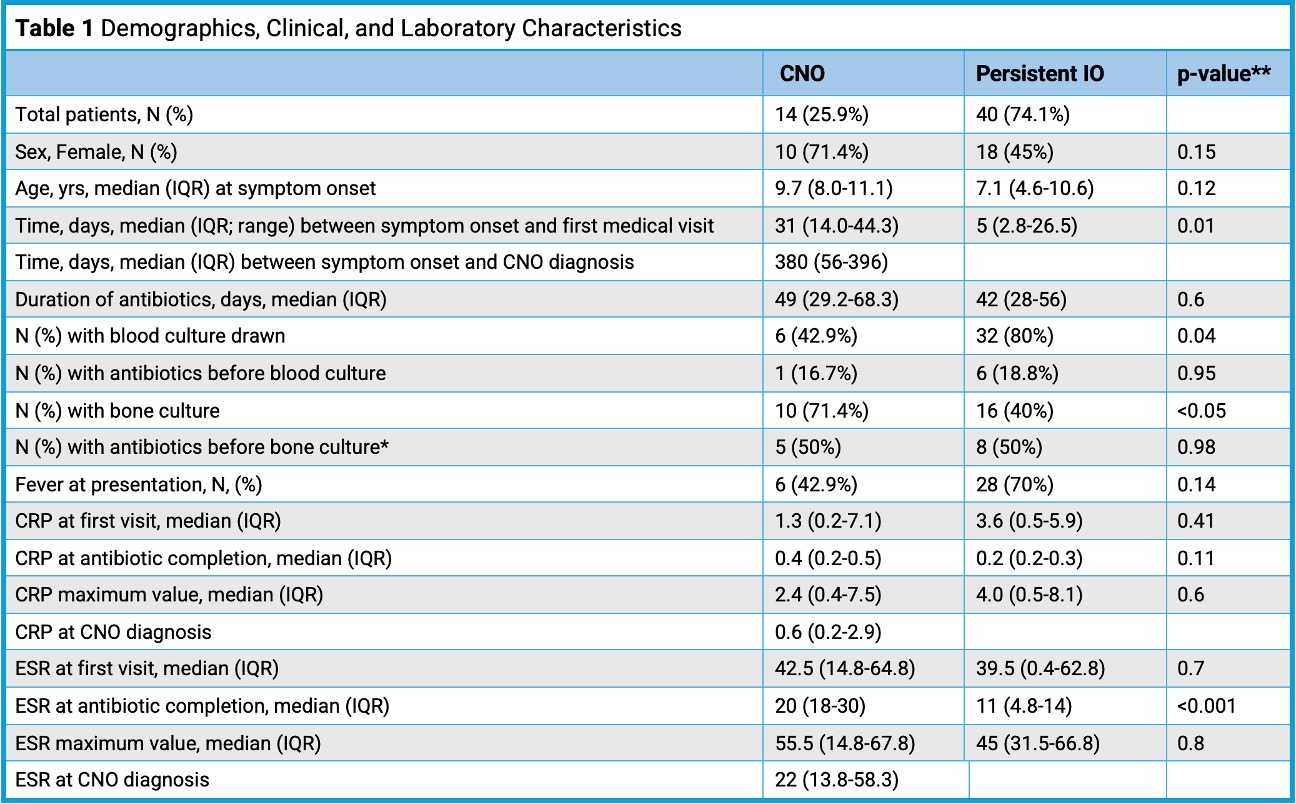
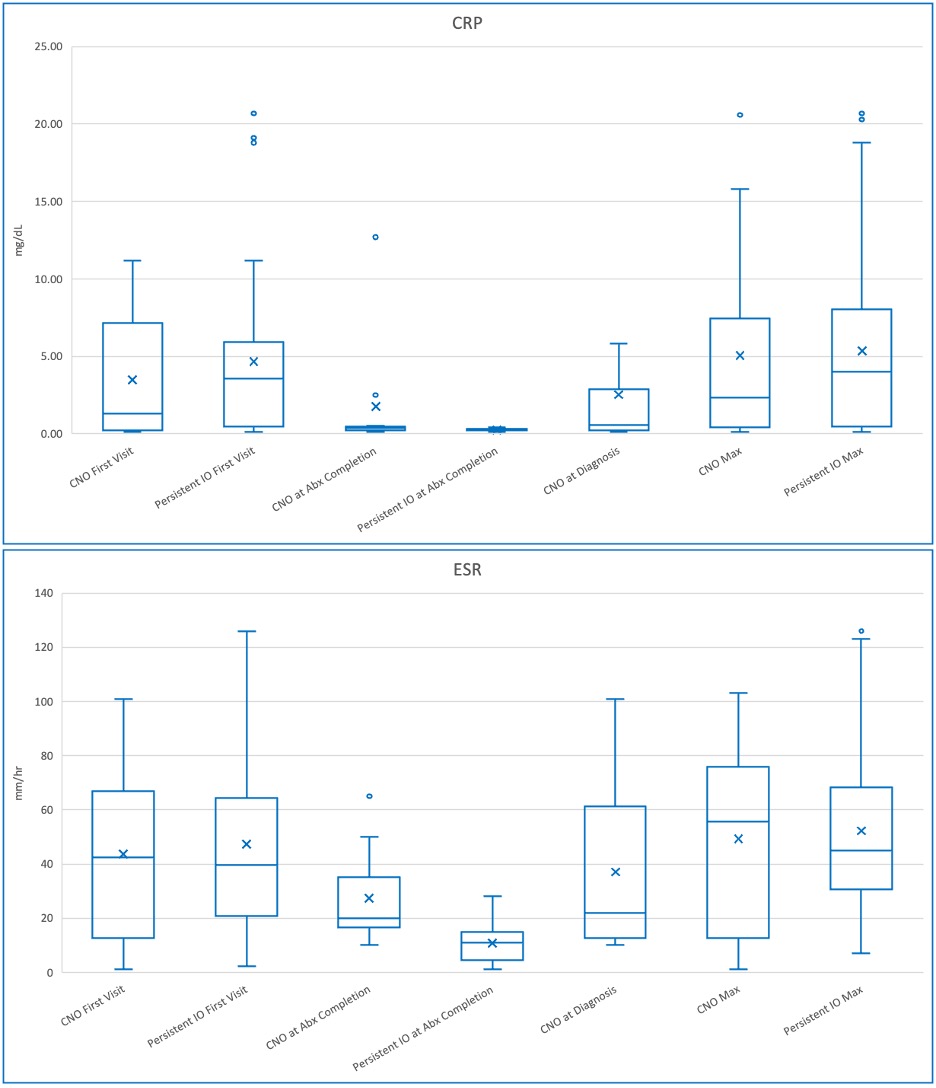
Results: Fifty-four patients were included in the analysis after a review of 617 patients’ charts. Of these, 14 (25.9%) were later diagnosed with CNO. The CNO cohort had a longer time between symptom onset and their first visit, were less likely to have fever at presentation, and had slightly lower CRP and ESR levels at their first visit (Table 1, Graph 1). Fewer patients in the CNO cohort had a blood culture (p=0.04), however, they were more likely to have a bone biopsy than those in the Persistent IO cohort. All patients received an empiric course of antibiotics. Median duration of antibiotics was similar between cohorts, and both had improvements in inflammatory markers with only ESR response to antibiotics reaching clinical significance (Table 1, Graph 1). Symptoms were less likely to respond in the CNO cohort (21.4% with no response, 42.9% with a partial response, and 35.7% with resolution of symptoms) vs. Persistent IO (12.5% with a partial response, 85% with resolution of symptoms) X2(2, N=54)=14.38, p=0.001.
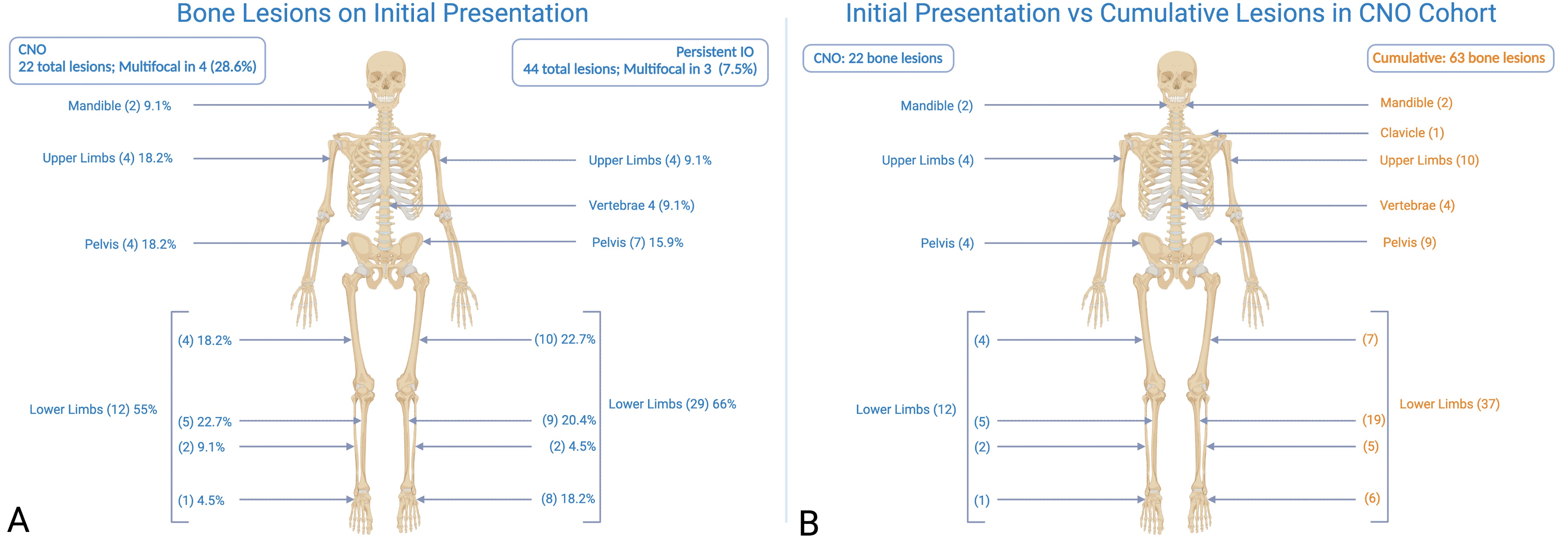
Lesions were distributed similarly at initial evaluation (Figure 1A). Among the 14 patients in the CNO cohort there were 22 total lesions at initial evaluation. An additional 41 lesions (65% of total CNO lesions) were later identified in this cohort using whole-body MRI (WB-MRI) (Figure 1B).
Conclusion: We did not identify robust distinguishing characteristics between the CNO and IO cohorts. CNO should remain on the differential for culture negative IO, as multifocal involvement may not be evident at presentation, highlighting the utility of WB-MRI. Additional research is needed to understand the pathophysiology of early CNO, and the possibility of infection triggering the development of CNO.
*One in each cohort had a bone biopsy much later than symptoms/diagnosis. In the CNO cohort one patient had a bone biopsy over 6 months after CNO diagnosis to confirm the diagnosis in light of new symptoms. In the Persistent IO group one had a bone biopsy 4 years later with no pathology found. These are excluded from the analysis.
** p-values calculated from Mann-Whitney-U-Test with a significance set at 0.5
To cite this abstract in AMA style:
Grim A, Zhao Y, Wang C, Janssen E, Turnier J, Hyrhorczuk A, Saad N. Relationship Between Culture Negative Infectious Osteomyelitis and Chronic Nonbacterial Osteomyelitis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/relationship-between-culture-negative-infectious-osteomyelitis-and-chronic-nonbacterial-osteomyelitis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-between-culture-negative-infectious-osteomyelitis-and-chronic-nonbacterial-osteomyelitis/