Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: People with rheumatoid arthritis (RA), psoriatic arthritis (PsA), juvenile idiopathic arthritis (JIA), and axial spondyloarthritis (axSpA) are at risk for poor COVID-19 outcomes, including Long COVID. Little is known about the impact of Long COVID on rheumatic disease activity, disability, and quality of life. We examined these associations in people with inflammatory arthritis and prior COVID-19.
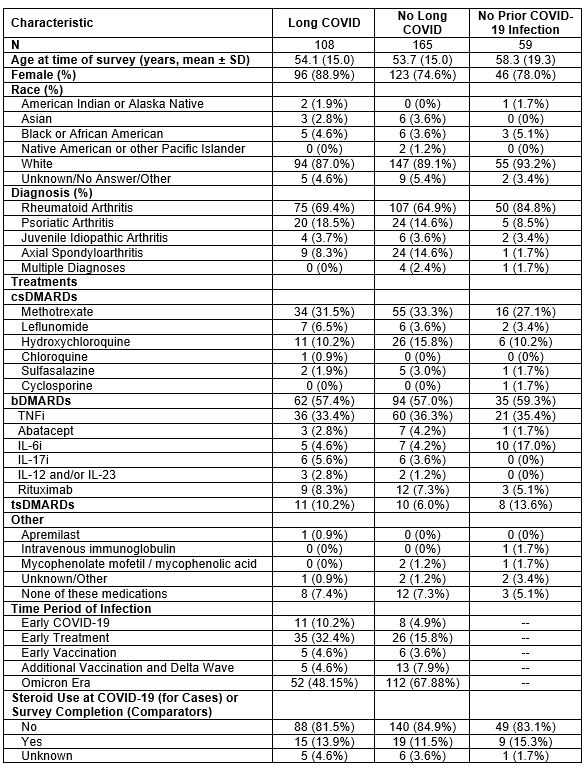
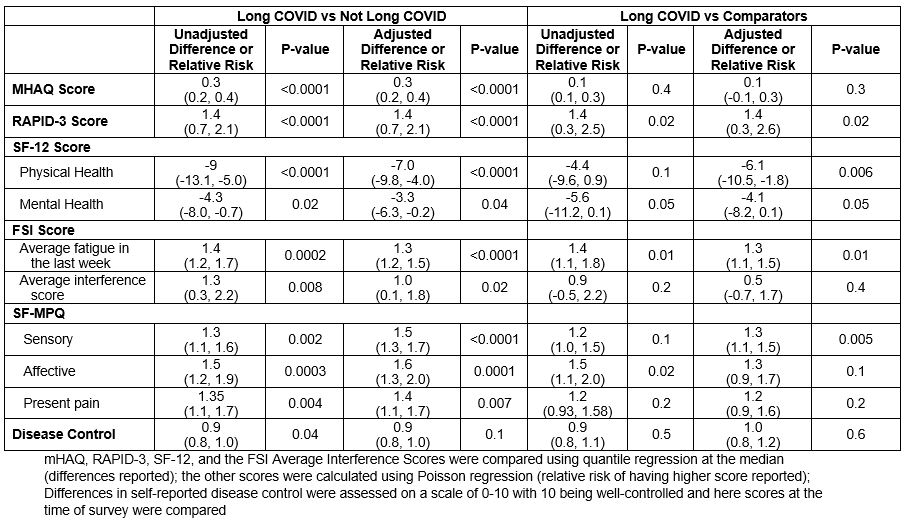
Methods: RheumCARD is a prospective cohort study recruiting people with systemic rheumatic disease with (≥ 28 days after COVID-19 onset) and without COVID-19 from a US healthcare system. Surveys include the Routine Assessment of Patient Index Data 3 (RAPID-3), modified health assessment questionnaire (MHAQ), short form 12 (SF-12), fatigue symptom inventory (FSI), and short form McGill Pain Questionnaire (SF-MPQ). Participants report rheumatic disease control (scale 0-10, 10 being well-controlled) before and after COVID-19 or test for COVID-19 (comparators). We included participants with inflammatory arthritis who did surveys 3/2021-10/2023. Participants reported symptoms that began with their infection and symptom duration. Long COVID was defined as symptoms of acute COVID-19 for ≥ 28 days (CDC Definition). We assessed the association of Long COVID with these measures in unadjusted and adjusted models.
Results: We analyzed n=108 with Long COVID, n=165 without Long COVID but prior infection, and n=59 without prior COVID-19 (Table 1). RA was the most common diagnosis (69.4%, 64.9%, 84.8%, respectively); most were female (88.9%, 74.6%, and 78.0%, respectively). Mean age was 54.1, 53.7, and 58.3 years, respectively. The most common Long COVID symptoms were fatigue/malaise (40.7%), altered or loss of sense of smell/taste (23.2% and 19.4%), congestion (17.6%), and cough (16.7%). Those with vs without Long COVID (Table 2) had worse mHAQ (median 0.4 vs 0.1, p< 0.01) and RAPID-3 (median 3.7 vs 2.3, p< 0.01) scores. They also had worse physical and mental health (median SF-12 component scores: 38.1 vs 47.2, p< 0.01 and 48.6 vs 53.0, p=0.03, respectively). They had greater fatigue and fatigue interference (median 5 vs 4, p=< 0.01 and 3.0 vs 1.7, p< 0.01) and worse sensory, affective, and present pain (p< 0.05 for all comparisons). Both groups rated worse control of their arthritis after vs before COVID-19 (P< 0.01 for each). Similar trends were observed when comparing those with Long COVID to those without prior COVID-19. These differences persisted after adjustment for age, sex, and race (Table 3) and after adjusting for baseline depression.
Conclusion: People with inflammatory arthritis and Long COVID have worse self-reported disease activity, quality of life, fatigue, and pain when compared to those who had COVID-19 but no Long COVID. The differences in several measures were greater than the minimally clinically important differences. These findings suggest that SARS-CoV-2 may trigger a process in some people with inflammatory arthritis that exacerbates pain and fatigue and reduces quality of life. Interpretation of patient-reported outcome measures, especially disease-specific measures, even months after COVID-19, may be difficult because of the impact of Long COVID.
To cite this abstract in AMA style:
Wallace Z, Lin M, Srivatsan S, King A, Wang X, Venkat R, Patel N, Kawano Y, Schiff A, Hanberg J, Kowalski E, Johnson C, Vanni K, Williams Z, Qian G, Bolden C, Mueller K, Bade K, Saavedra A, Sparks J. The Impact of COVID-19 and ‘Long COVID’ on Self-Reported Disease Activity, Disability, and Quality of Life in Patients with Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-covid-19-and-long-covid-on-self-reported-disease-activity-disability-and-quality-of-life-in-patients-with-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-covid-19-and-long-covid-on-self-reported-disease-activity-disability-and-quality-of-life-in-patients-with-inflammatory-arthritis/