Session Information
Date: Saturday, November 16, 2024
Title: Imaging of Rheumatic Diseases Poster I: Inflammatory Arthritis
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The musculoskeletal involvement in psoriatic arthritis (PsA) can involve both articular and extra articular structures manifested by inflammatory and structural lesions. The relationship between tender and/or swollen joints and these lesions detected in imaging is not clear.
Aim: To examine the significance of tenderness with or without swelling of PsA finger joints in relation to inflammatory and structural findings on magnetic-resonance-imaging (MRI), ultrasound (US) and X-ray.
Methods: The current study included prospectively recruited 100 PsA patients (CASPAR criteria) with a history of finger joints involvement. The physical exam categories included: Tender and swollen joints (TJ and SJ), Tender not swollen joints (TJ not SJ), not tender and not swollen joints (not TJ and not SJ). Swollen not tender joints was excluded due to paucity of findings (only 3 joints). On the same day of the clinical evaluation, all the patients completed US assessment (gray scale and Doppler) of 14 finger joints of the more symptomatic hand. Sonographic synovitis, flexor tenosynovitis, extensor peritenonitis, erosions and bone proliferations were assessed and scored according to the definitions and scoring systems of the EULAR-OMERACT. Within 3 days, all the patients completed MRI of this hand assessing and scoring synovitis, flexor tenosynovitis, periarticular inflammation, BME, erosion and bone proliferation according to the PsAMRIS method. Within 1 month, 70 patients completed X-ray of this hand assessing and scoring erosions and bone proliferations according to the Psoriatic Arthritis Ratingen Score method. The US, MRI and X-ray readers were blinded to the clinical data.
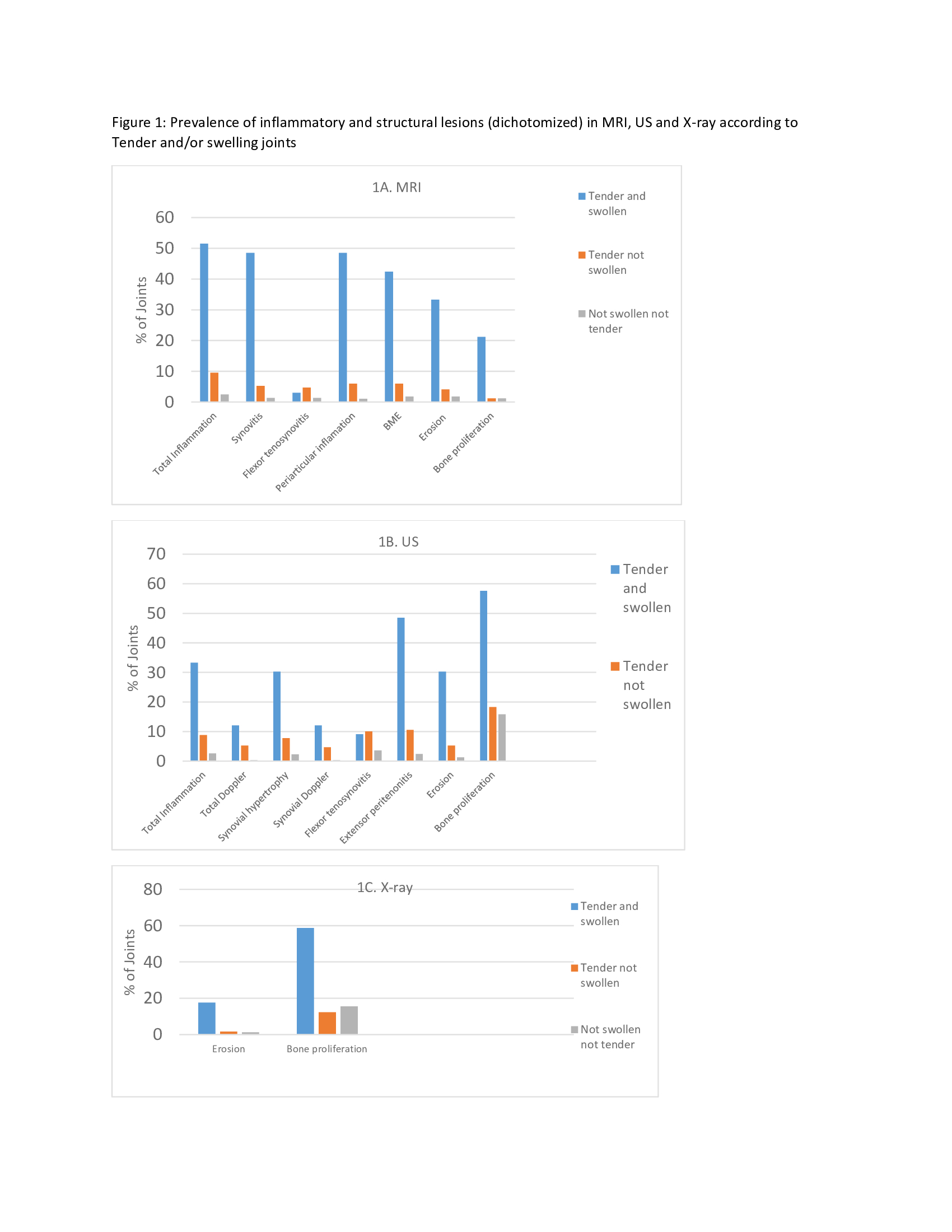
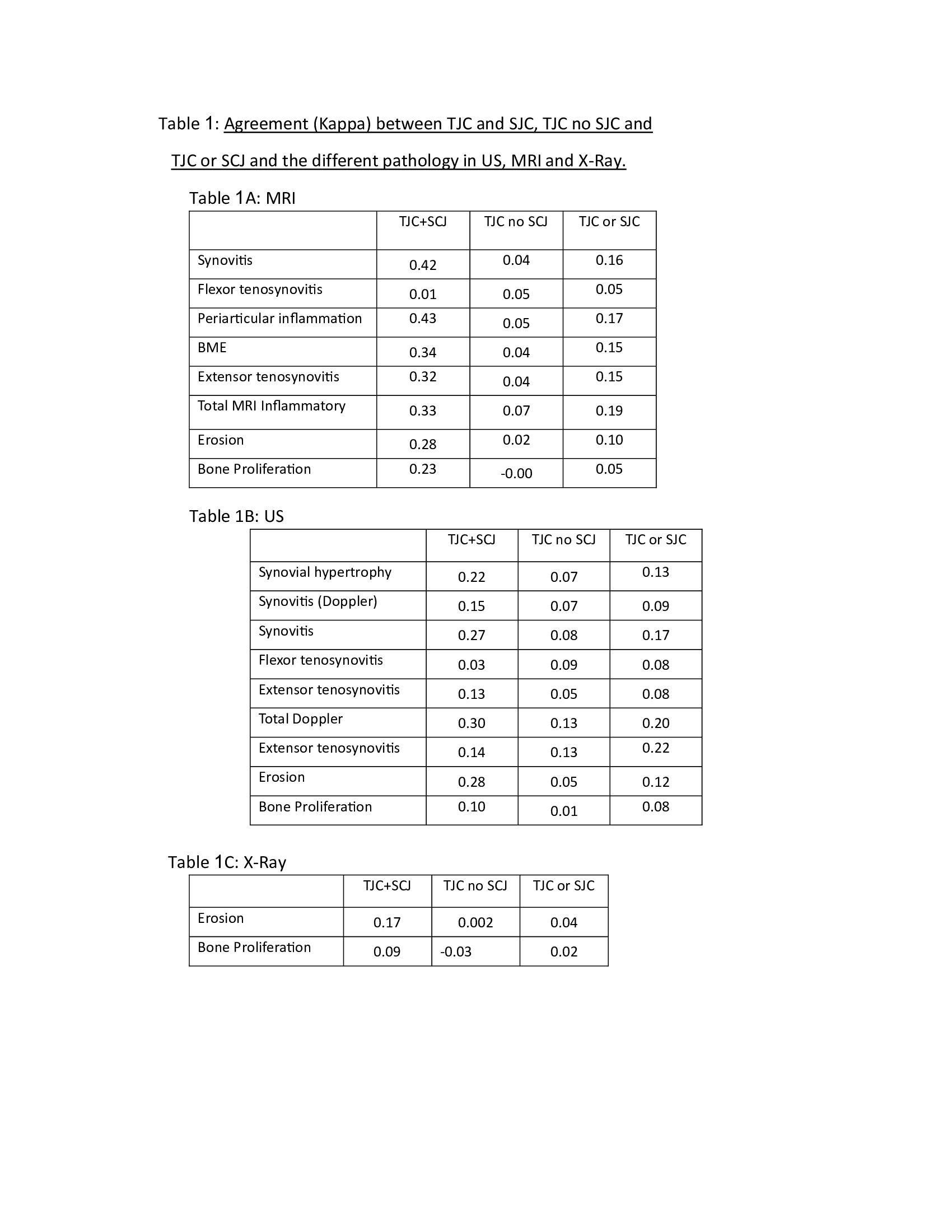
Results: The mean age was 51.2 (± 12.6), 59% were females and the mean PsA disease duration was 10.3 (±11.2) years. The TJ and SJ category had the highest prevalence of inflammatory and structural lesions in MRI, US and x-ray (figure 1). However, 49.5% and 66.6% of the patients in this category had no inflammatory finding (signified in figure 1 as total inflammation) in MRI and US, respectively. The TJ not SJ category had a substantially lower prevalence of lesions in all imaging modalities compared to the TJ and SJ category, but had higher prevalence than not TJ and not SJ category. The agreement between the TJ and SJ and MRI and US ranged between slight to moderate (kappa 0.01 and 0.03 for tenosynovitis to 0.42 and 0.27 for synovitis in the MRI and US, respectively), while the agreement (kappa) between the TJ not SJ were lower, all in the slight agreement category (Table 1).
Conclusion: The agreement between physical examination and MRI, US and X-ray in PsA was weak. TJ and SJ were related to the highest prevalence of inflammatory lesions, however the specificity was low, emphasizing the importance of imaging in this category. TJ without SJ had low prevalence of inflammatory lesions suggesting low level of significance. Patients without TJ and SJ did not have evidence of subclinical inflammation.
TJC or SCJ and the different pathology in US, MRI and X-Ray
To cite this abstract in AMA style:
Furer V, Eshed i, iluz M, Elkayam O, Polachek A. The Significance of Tenderness with or Without Swelling of Finger Joints in Relation to Magnetic-resonance-imaging, Ultrasound and X-ray in Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-significance-of-tenderness-with-or-without-swelling-of-finger-joints-in-relation-to-magnetic-resonance-imaging-ultrasound-and-x-ray-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-significance-of-tenderness-with-or-without-swelling-of-finger-joints-in-relation-to-magnetic-resonance-imaging-ultrasound-and-x-ray-in-psoriatic-arthritis/