Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Mortality due to cardiovascular disease, infections, and renal disease is elevated in people with systemic lupus erythematosus (SLE) compared with the general population, but to our knowledge, no studies assessed SLE as an underlying or contributing cause of death based on death certificates in the US.
Methods: We examined SLE as an underlying and contributing cause of death using 2018–2022 mortality data in CDC WONDER for persons aged ≥15 years, overall and by age, sex, race/ethnicity, and geographic region. SLE deaths were identified using the International Classification of Diseases, Tenth Revision (ICD-10) code M32. Crude and age-adjusted (standardized to the 2000 U.S. standard population) mortality estimates per 100,000 population with 95% confidence intervals (CIs) were calculated. Non-overlapping 95% CIs were considered statistically significant to examine differences by demographic characteristics.
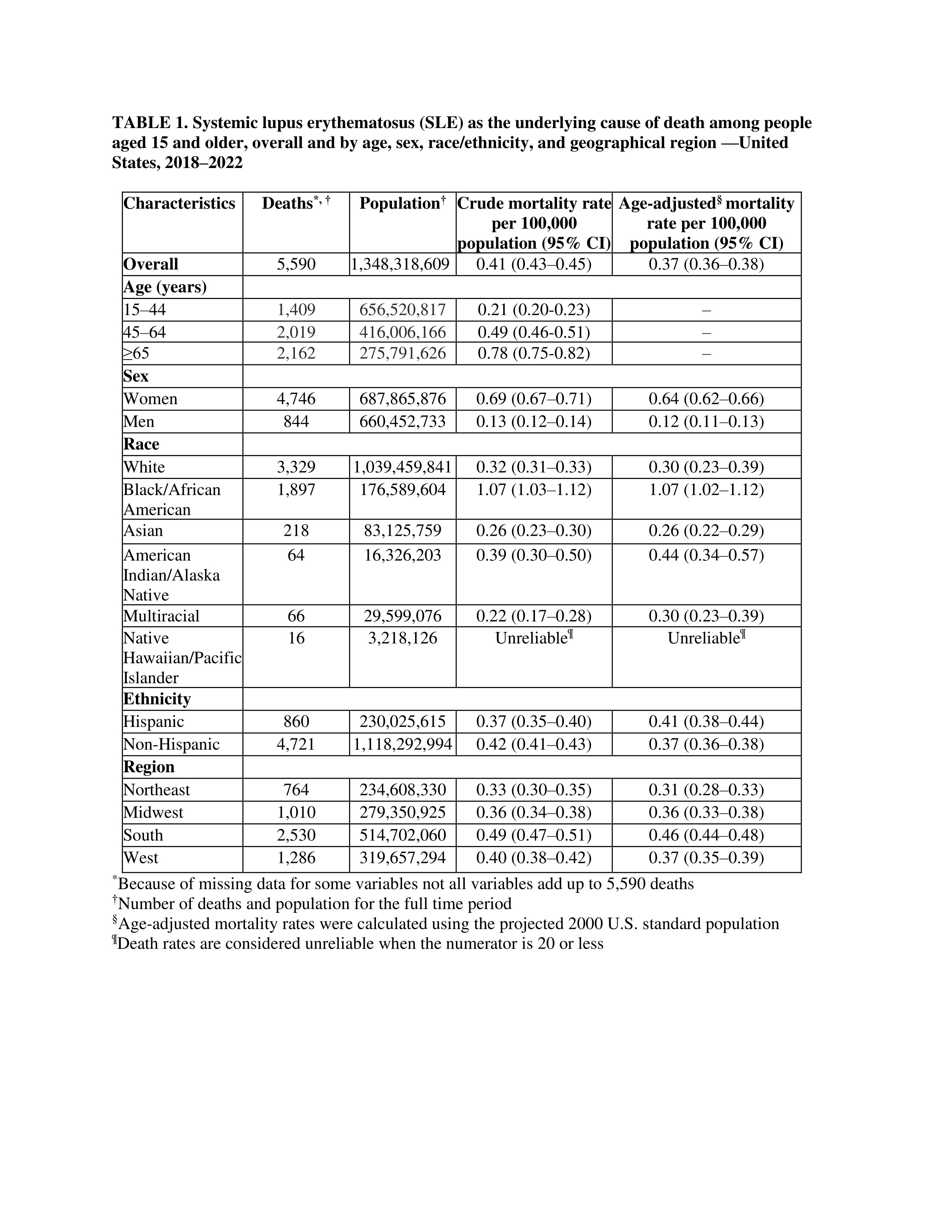
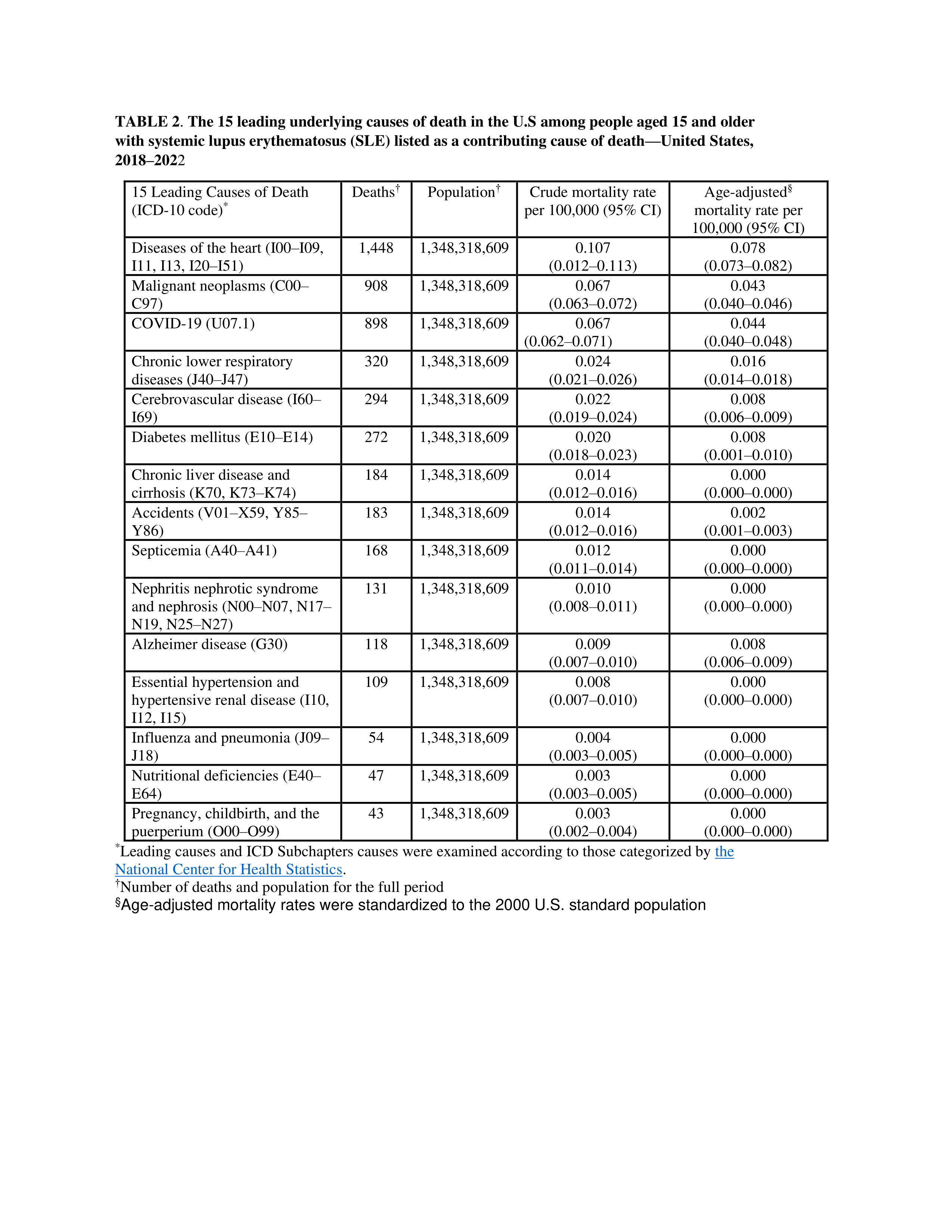
Results: For the period 2018–2022, 12,645 deaths listed SLE as either an underlying or a contributing cause of death (crude rate per 100,000=0.94). Of these deaths, 5,590 (44%) listed SLE as the underlying cause of death (crude rate=0.41). Age-adjusted mortality rates for SLE as an underlying cause of death (Table 1) were greater in women (rate=0.64) than men (0.12), Black/African Americans (1.07) versus other race/ethnic groups (range=0.26–0.44), Hispanics versus non-Hispanics (0.41 versus 0.37), and in the South (0.46) versus other regions (range= 0.31–0.37). The age-adjusted rate was highest for Black/African American women [1.78 (95% (CI:1.69–1.87)]. Where SLE was listed as a contributing cause of death, the leading underlying causes of death (age-adjusted) were diseases of the heart (rate=0.08), malignant neoplasms (rate=0.04), and COVID-19 (rate=0.04) (Table 2).
Conclusion: Results identified racial, ethnic, and geographic disparities in SLE mortality. The leading underlying causes of death where SLE was listed as a contributing cause of death were highest for diseases of the heart, but also substantial for COVID-19 and malignant neoplasms. These data can be used to understand the burden of SLE mortality in the US and to inform strategies and public health interventions to reduce SLE mortality in the population.
To cite this abstract in AMA style:
Dawson D, Greenlund K, Barbour K. Systemic Lupus Erythematosus Mortality—United States, 2018–2022 [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/systemic-lupus-erythematosus-mortality-united-states-2018-2022/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-lupus-erythematosus-mortality-united-states-2018-2022/