Session Information
Date: Tuesday, November 14, 2023
Title: Abstracts: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: Recent studies suggest that post-fracture pharmacologic management has been declining in the U.S. despite an increase in the burden of osteoporosis (OP). In light of this treatment gap, few studies have reported on the incidence of subsequent fracture risk among commercially insured postmenopausal women with a history of fracture.
Methods: We assembled a retrospective cohort of women aged ≥50 years from 2012-2021 using an administrative claims database of privately insured or employer-sponsored Medicare Advantage coverage. Osteoporotic fractures were identified by ≥1 insurance claims with a relevant diagnosis and/or procedure code for an open or closed fracture. Treatments for osteoporosis were identified by prescription fills or medical procedure claims. The cumulative incidence of a new, subsequent fracture at the same or a different anatomic site was estimated for any (clinical vertebral, hip, femur, pelvis, tibia, fibula, radius/ulna/distal forearm, humerus, clavicle, rib, sternum), major (any fracture excluding extremities, clavicle, rib, sternum), hip, and clinical vertebral fractures occurring ≥90 days of initial index fracture to up to 2 years. Women were followed from the index fracture for up to 2 years to estimate the cumulative incidence of any treatment uptake. All analyses used inverse probability weighting to adjust for differential censoring due to differences in demographics and clinical risk factors.
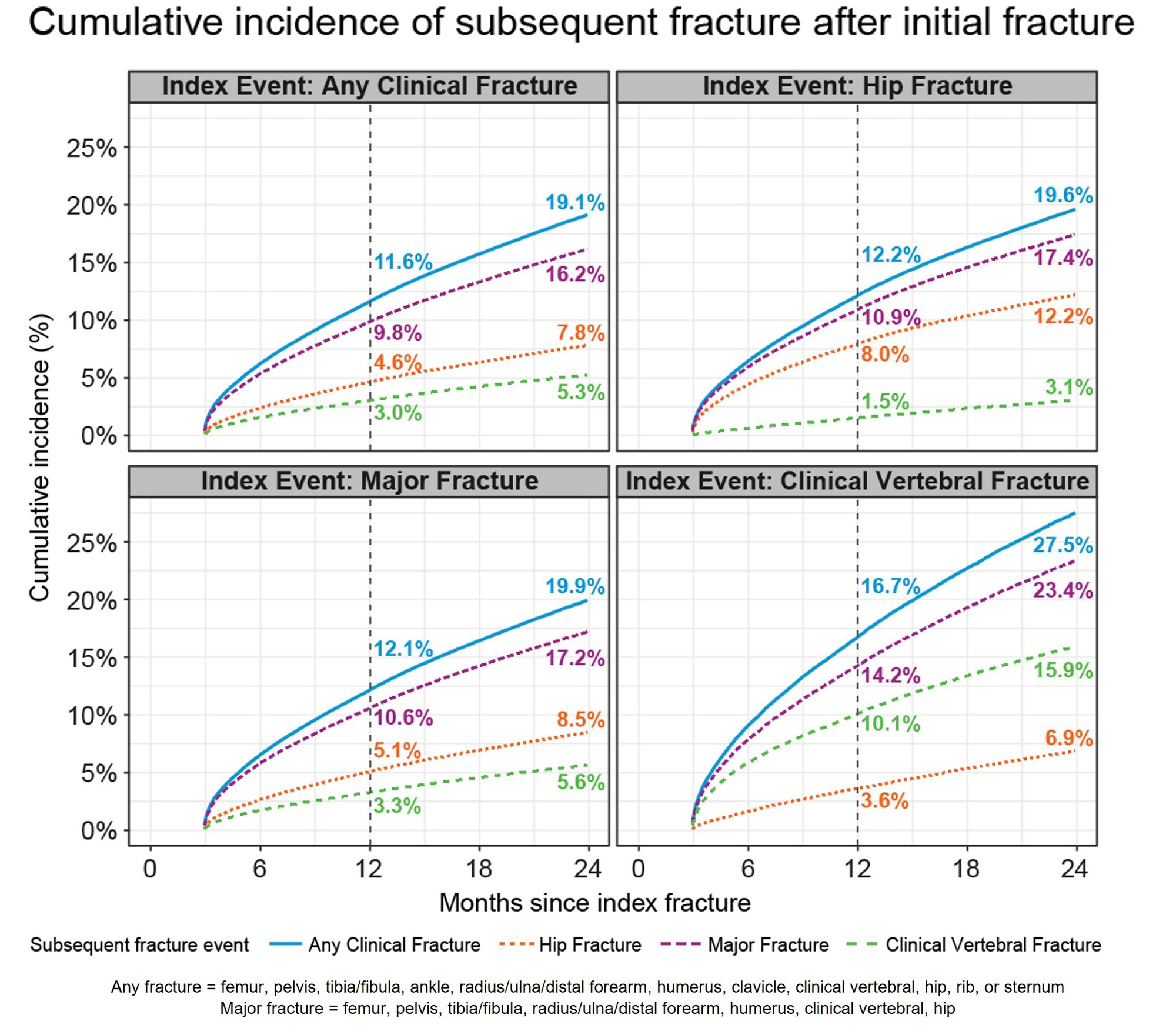
Results: Among the 483,564 women with any initial fracture (mean age 74.8), the 1-year cumulative incidence of a subsequent fracture at any site was 11.6%, which increased to 19.1% at 2 years (Figure). The same-site subsequent fracture risk was highest for women with an initial clinical vertebral fracture: 10.1% experienced a subsequent vertebral fracture at year 1 and 15.9% at year 2. Among women with an initial hip fracture, 12.2% and 19.6% experienced a subsequent fracture at any site after 1 and 2 years, respectively, while 8.0% and 12.2% experienced a subsequent hip fracture at 1 year and 2 years, respectively. Most patients did not receive pharmacological treatment one year (91.7%) and two years (89.4%) after their initial fracture.
Conclusion: Although clinical guidelines specify that OP is a lifelong, chronic disease requiring ongoing management, recent data over a 10-year period show that recurrent fracture rates within 2 years are high, while pharmacological treatment remains underutilized in this high-risk population.
To cite this abstract in AMA style:
Kim M, Brunetti V, Cosman F, Curtis J, Lewiecki E, Phelan M, Samai P, McDermott M, Lin T, Brookhart M, Hurwitz K. Current Trends in the Risk of Subsequent Fracture After Initial Fracture, and Post-Fracture Treatment Among Commercially Insured Postmenopausal Women in the United States [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/current-trends-in-the-risk-of-subsequent-fracture-after-initial-fracture-and-post-fracture-treatment-among-commercially-insured-postmenopausal-women-in-the-united-states/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/current-trends-in-the-risk-of-subsequent-fracture-after-initial-fracture-and-post-fracture-treatment-among-commercially-insured-postmenopausal-women-in-the-united-states/