Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
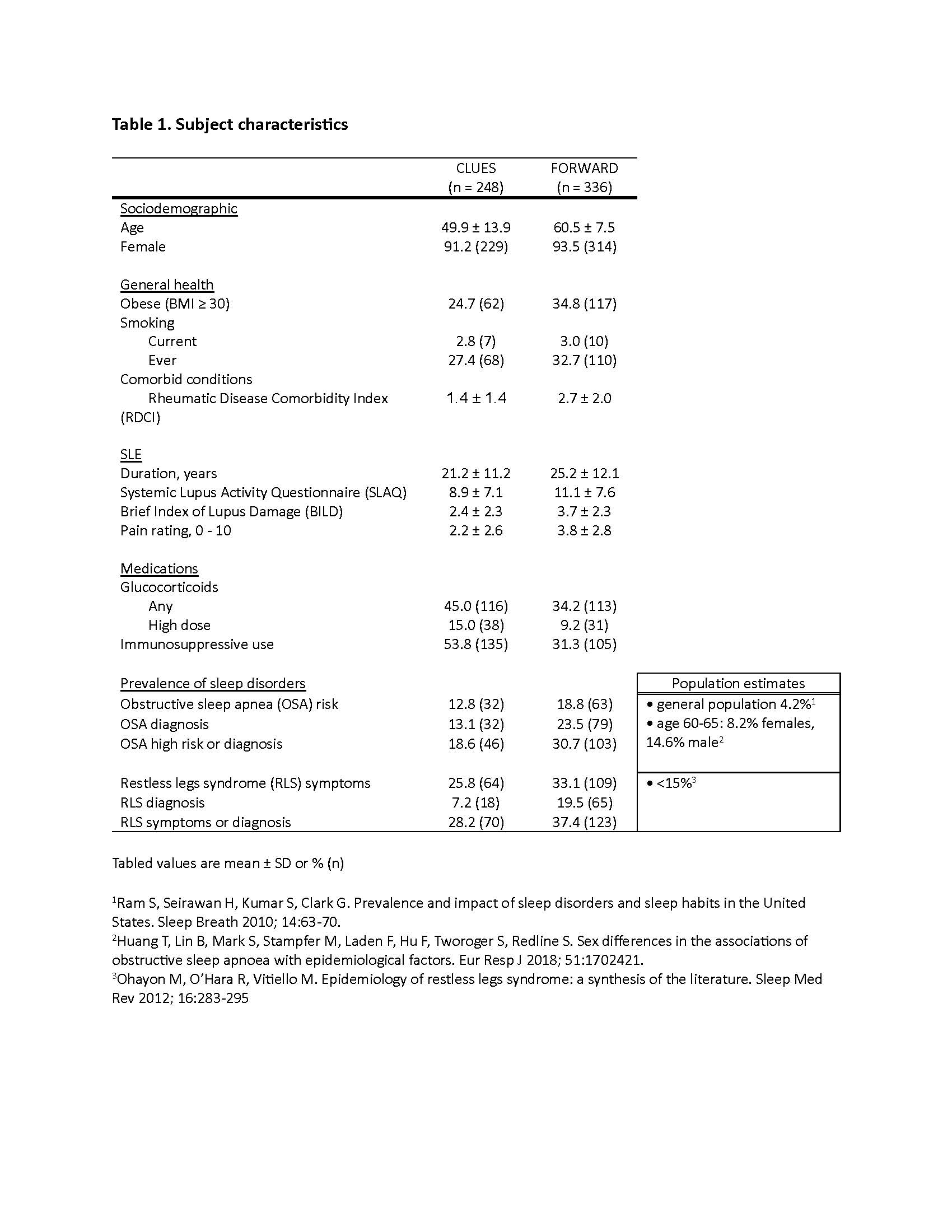
Background/Purpose: Research in the general population has linked sleep disorders to poor outcomes such as lower pain thresholds, fatigue, cognitive impairment, depression, and cardiovascular disease – important health outcomes relevant to lupus, as well as higher levels of systemic inflammation, which may influence SLE disease activity and symptoms. SLE-specific studies have linked self-reported sleep problems with greater disease activity and symptoms and even risk of lupus onset. Some sleep disorders are more common among older individuals. We examine the prevalence of self-reported sleep disorders in two SLE cohorts, one with greater representation from older adults with SLE.
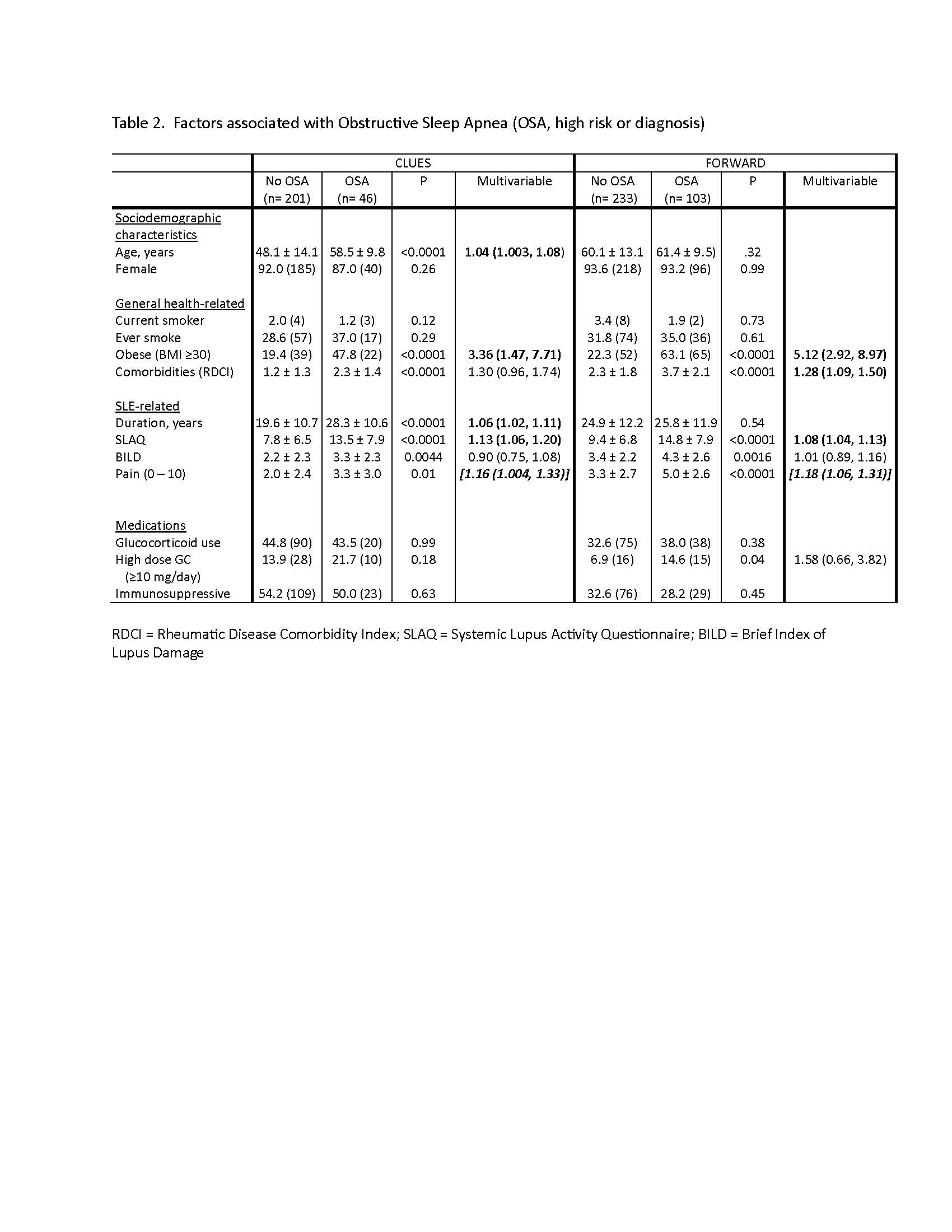
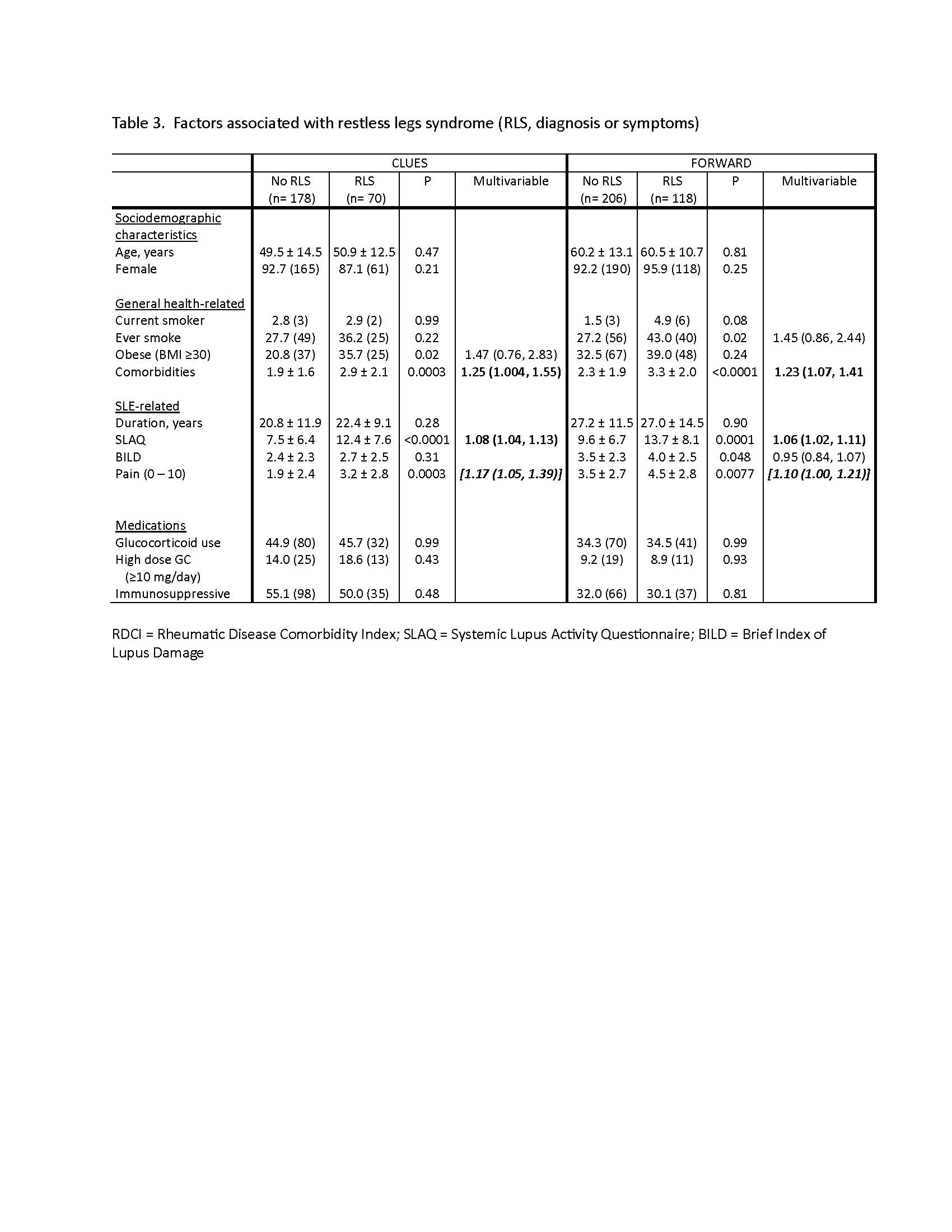
Methods: Data are from participants with physician-confirmed SLE in the California Lupus Epidemiology Study (CLUES) and the FORWARD Databank. In one data collection period in each study, we examined two sleep disorders: obstructive sleep apnea (OSA) using the validated STOP-Bang questionnaire and self-reported OSA diagnosis, and restless legs syndrome (RLS) using validated self-reported questions and self-reported RLS diagnosis. We examined the prevalence of OSA and RLS and the overlap between the two in each cohort. Unadjusted analyses identified significant associations between OSA and RLS and sociodemographic (age, sex, income, education), general health (smoking, obesity, comorbidities [Rheumatic Disease Comorbidity Index, RDCI), and SLE-related (SLE duration, self-reported disease activity [Systemic Lupus Activity Questionnaire, SLAQ], and damage [Brief Index of Lupus Damage, BILD], 0-10 pain rating, glucocorticoid use, use of immunosuppressive medications) characteristics. Multivariable analyses to identify independent associations of sleep disorders included all variables significant at p≤0.10 in unadjusted analyses.
Results: Mean age was 50 ± 14 years in CLUES and 61 ± 12 years in FORWARD (Table 1). Prevalence of each sleep disorder was higher in the older FORWARD cohort and considerably higher in both cohorts than in the general population (Table 1). In CLUES and FORWARD, 36.7% and 53.8% of participants, respectively, had at least one sleep disorder. In multivariable analyses, SLAQ, pain, and a higher number of comorbid conditions were the most consistent factors associated with sleep disorders (Tables 2 and 3).Obesity (BMI ≥30 kg/m2) was also associated with OSA.
Conclusion: High proportions of individuals in both of these SLE cohort had sleep disorders; prevalence was greater in the older cohort. Factors associated with sleep disorders – comorbid conditions, disease activity, and pain – were similar in the two cohorts. Given the association of sleep disorders with poor health outcomes, increased awareness of and screening for sleep disorders among SLE patients may be beneficial, particularly among older adults who may be more likely to have sleep disorders and be more sensitive to the negative impacts of sleep disorders.
To cite this abstract in AMA style:
Katz P, Dall'Era M, Yazdany J, Michaud K. Self-Reported Sleep Disorders Among Individuals with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/self-reported-sleep-disorders-among-individuals-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-reported-sleep-disorders-among-individuals-with-systemic-lupus-erythematosus/